Find out more
Find out more about what Academic Health Science Networks (AHSNs) are doing to tackle inequalities in maternity care.
Find out moreWomen and birthing people from black, Asian, or mixed ethnic backgrounds are significantly more likely to experience poor outcomes during their maternity journey. Between September 2021 and October 2022, Darzi Fellow Rosie Murphy undertook work in Croydon to explore these inequalities and what could be done to improve local services. This is the first in a series of blogs reflecting on the learnings and experiences from her Fellowship. Read Rosie's second blog focusing on key recommendations from the project and third blog focusing on the challenges of tackling structural issues during fixed-term projects.
Evidence points to a shocking disparity in maternal and perinatal death, preterm birth and fetal growth restriction, between people from black, Asian and mixed ethnic backgrounds and their white counterparts. This has a significant impact on health and economic outcomes, and while the causality is not fully understood there has previously never been a policy ambition designed to address this.
However, following the health inequalities highlighted by the Covid-19 pandemic and the impact of the Black Lives Matter movement, this is starting to change. In September 2021, NHS England requested each local maternity and neonatal system develop a strategy to address this by September 2022.
In Croydon, work to improve outcomes for women from minoritised ethnic backgrounds was underway before this. The maternity unit delivers 3,200 babies per year and approximately 52 per cent of Croydon residents are from minoritised ethnic backgrounds, which is representative of the maternity population.
In Spring 2021, a passionate and dedicated midwife, Olamide Odusanwo, was determined to do what she could to tackle the issue of perinatal inequality. With colleagues Gina Short, Helen Chambers and Ranee Thakar, she set up the HEARD (Health Equity And Racial Disparity) campaign.
They carried out surveys with women (and birthing partners) and staff to better understand the local context. This led to changes including increased appointment length and frequency for people from minoritised ethnic backgrounds, and the creation of a dedicated service for people who felt their concerns were not being heard during their maternity journey. They also helped identify the scale of work needed to tackle the issue and the clear need for a dedicated midwife to work on the project.
This is where I came in – a midwife by background, with a passionate interest in health inequalities – I came to Croydon as part of the Darzi fellowship leadership programme. The Darzi fellowship includes a PGCert Leadership in Healthcare and a change project in the hosting trust. We are expected to explore the challenge in depth to develop long term, sustainable solutions.
To scope the project we interviewed a number of stakeholders including women and birthing partners from minoritised ethnic backgrounds, as well as voluntary sector staff involved in related health equity projects. The most common themes were access, barriers and listening to women and birthing people.
We looked for data which could help illustrate these three themes. However, data on ethnicity is poorly recorded which made it difficult to establish a baseline. While work is ongoing at a national level to address this (NHSEI 2021), it was a significant limitation to the project. We also struggled to find data to illustrate the themes of listening to service users and barriers. However, the theme of not listening to women and birthing people was identified in the preliminary Ockenden report where recommendations were made about the need to improve this.
Due to its complexity the issue was quickly identified as a ‘wicked’ problem. Wicked problems need to be addressed using a collective approach. This is because no individual perspective is enough and so solutions must be built on collective knowledge. Accordingly, there was a clear need to develop a ‘collective’ to undertake the work by creating a network.
We hosted a Whose Shoes event to engage interested citizens and wider health and voluntary sector staff, to establish a network and start discussing solutions. Whose Shoes is an award-winning board game with a multi-perspective approach to transforming health and social care services by putting the person in the centre. It is renowned for its co-production ethos and has a strong track record in maternity care.
It was crucial for us to reach groups beyond those normally reached by our engagement work. As part of this we had to overcome mistrust of institutions, which we started to address by holding the event at a trusted voluntary sector partner organisation - Croydon BME Forum - instead of on hospital premises. We sent invitations via social media from this organisation, the Asian Resource centre Croydon, Happy Baby Community and Big Local Broad Green.
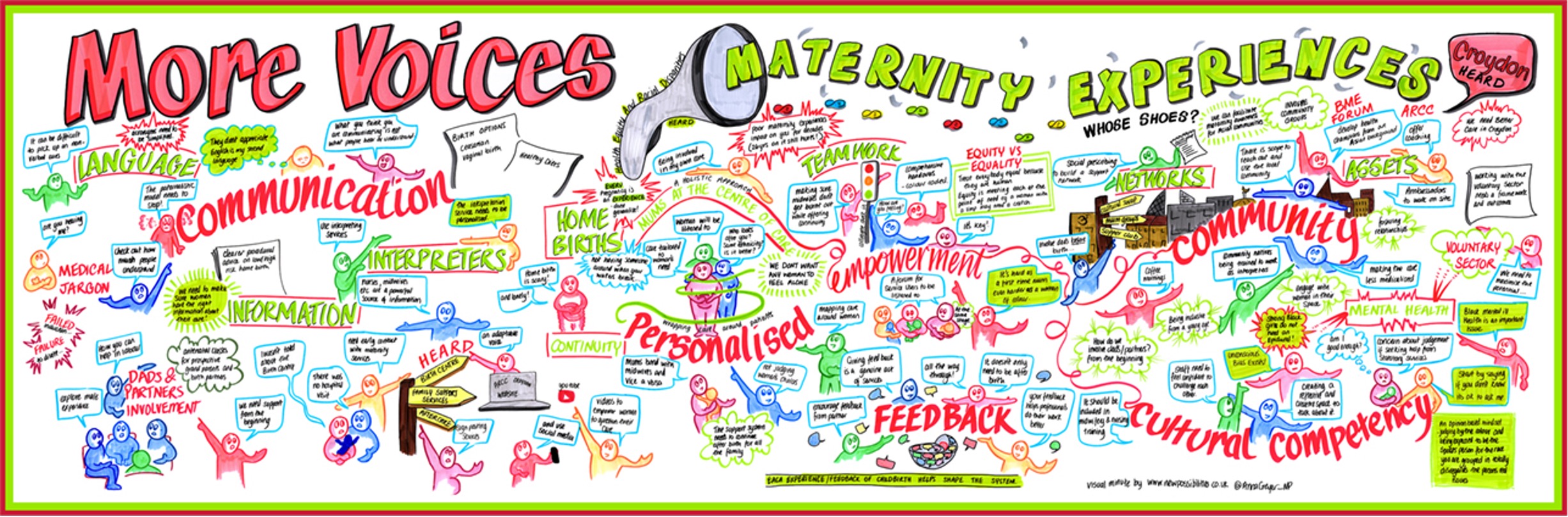
The event was well attended and resulted in us expanding the membership of the HEARD campaign to include local experts by experience (women and birthing partners) and wider health and voluntary sector members. This was key for co-design of the next steps. The picture board below recaps the informal discussions that were had during the Whose Shoes event, highlighting the topics that members felt were important to address.
As is often the case with fixed-term projects, it feels like we are really starting to gather momentum, just as my year is coming to an end. Nevertheless, the brilliant work of the HEARD campaign will continue after the completion of my Darzi fellowship and as I leave, I am acutely aware of the power of people. This project started with one idea from one midwife, who shared her idea with others, who in turn shared it with more people who then all came to coalesce around the same cause - to drive the change they wanted to see in their community.
With enormous thanks to Ranee Thakar, Gina Short, Olamide Odusanwo, Manjit Roseghini, Donnarie Goldson, Mobola Jaiyesimi, Antoinette Johnson, Leila Howe, Gemma Dakin, Alison White, Jay Patel, Ima Miah, Felisha Dussard, Andrew Brown, Tai Lamard, Gill Phillips, Paul Macey and all the birthing families of Croydon who were so generous in sharing their experiences with me.
Find out more about the maternity and neonatal work happening in South West London ICS.

Find out more about what Academic Health Science Networks (AHSNs) are doing to tackle inequalities in maternity care.
Find out more