Welcome to the review of our year in 2021/22
"The impact of the pandemic has accelerated innovation in many health and care settings and our work has never been more important."
Dr Rishi Das-Gupta, Chief Executive
Introduction
Welcome to our Annual Report for 2021/22. The work of the HIN during this year has been a mixture of our long-term priorities and supporting our local system with short term challenges due to the pandemic. I am very proud that our team have risen to the challenge.
The vaccines and booster roll-out was an incredible national effort led by our amazing health and care professionals that showcased what can be achieved when we work together.
However, Covid-19 continued to touch every community across the country and left huge health and care challenges, including the long waiting times to access care. In my view these have exacerbated health inequalities across our region.
Against this backdrop I am proud of what the HIN has achieved with our partners in my first year as CEO.
The impact of the pandemic has accelerated innovation in many care settings and our work to spread innovation in health and care has never been more important.
Whether evaluating the effectiveness of virtual wards, remote consultations in mental health or fast track hubs for minor operations, we are helping our partners learn lessons for the future as they tackle growing waiting lists.
We are helping ensure many more people benefit from cutting-edge technology, products and initiatives including a new asthma diagnostic device and a non-invasive procedure for patients with suspected coronary artery disease.
And we continue to support innovators to drive forward exciting and game-changing solutions to some of the biggest health and care challenges. From apps to AI and from community sports for people with learning disabilities to a bowel disease self-management tool we are helping to make a real difference to health outcomes.
Of course, we cannot do this important work on our own and I would like to pay tribute to all our health and care partners as well as the many innovators who we have worked with this year.
I am proud of the HIN team for its incredible efforts during another challenging but successful year. We continue to support them through our training programme (the HIN Academy), a comprehensive Health and Wellbeing programme ranging from meditation sessions to craft workshops and initiatives celebrating key events like Black and LGBTQ+ History Months.
We are well placed to build on our successes over the coming year, focusing efforts on new strategic priorities to address health inequalities, improve outcomes for people living with long term conditions and support innovators while evaluating innovation in real world settings. And we will continue to celebrate our diversity and help ensure the HIN continues to be a happy and joyful place in which to work.

Chief Executive
I was absolutely delighted to join the HIN this year as its Chair. Before my appointment I was already well aware of the HIN’s track record for strong collaboration with its partners and its staff’s reputation for professionalism and energy in delivering solutions to complex challenges.
I have now seen this first hand and I have really been struck by the range of projects the HIN is driving forward with partners against the backdrop of challenges across the health and care landscape - not least those created by Covid-19. This is testament to both its leadership and the skill and expertise of its staff.
In my short time here I have had the pleasure to meet many of our partners who have praised the collaborative nature of the HIN and its expertise in pioneering fields such as Artificial Intelligence and remote technologies.
I have also met a wide range of fellow AHSN Chairs and other colleagues across the Network. It has been great to hear how HIN is working in partnership to deliver key national priorities such as early interventions for eating disorders and accelerating the adoption of innovative products designed to improve patient care and health outcomes.
This Annual Report sets out the breadth of this work and the difference it is making to communities across south London and beyond.
All of this means we are well placed to meet the challenges ahead while also harnessing the many opportunities.
The introduction of Integrated Care Boards will radically reshape the health and care landscape and our unique relationship with local partners mean we are in a strong position to ensure innovation is centre stage of their work.
We are already leading national programmes and delivering others. The way we work with the AHSN Network will be crucial in spreading innovation nationally so we can ensure the whole country benefits.
We are at the early stage of the convergence between health and data which will help deliver better health outcomes. I am keen to use my commercial experience to help drive forward even more projects that can exploit the latest technologies in key growth areas like smartwatches, as the use of data science in health and innovations such as wearable technology have so much potential to transform healthcare and outcomes for people, particularly for those living with long term conditions.
I am delighted to be part of the HIN at such an exciting time.

Chair
Accessing innovations
Supporting African and Caribbean communities at risk of type 2 diabetes
Healthy Eating and Active Lifestyles for Diabetes (HEAL-D) is a culturally tailored health programme for people from African and Caribbean communities who are at greater risk of developing type 2 diabetes.
This year we continued to work closely with partners to support the remote delivery of HEAL-D during Covid-19, with 76 people taking part in remote sessions.
We were delighted that, in partnership with the South London Applied Research Collaborative (ARC), we were awarded funding to further evaluate the effectiveness of HEAL-D and prepare it for rapid scale up across the country.
We also supported a successful transition of the HEAL-D referral process to the Diabetes Book & Learn platform ensuring that all eligible south London residents have access to the programme.
A further 10 HEAL-D courses have been confirmed for 2022/23.
HEAL-D attendee
Helping to identify and treat people with high cholesterol
High cholesterol is one of the major underlying causes of cardiovascular disease (CVD), which in turn causes 27 per cent of deaths in the UK. This year we have continued to work with partners to ensure the south London population benefits from new and established treatments to manage their cholesterol and reduce risk from cardiovascular events like heart attacks and stroke. This has involved identifying patients at greatest risk and optimising their treatment with the right medicines or lifestyle advice through implementation of an evidence-based lipid management pathway.
In south east London we have supported local commissioners to:
- Deliver three educational webinars to more than 250 primary care healthcare professionals involved in lipid management.
- Revise and launch their Lipid Management Pathway.
- Identify six Primary Care Network test beds and hold monthly Community of Practice meetings with them to inform practice and share learning
In south west London we supported the ICS to secure over £100,000 to:
- Recruit a clinical pathfinder to upskill primary care clinicians, deliver quality improvement sessions and streamline the referral pathway.
- Deliver point of care testing in community settings such as places of worship, sporting events and shopping centres.
- Support primary care providers in proactively identifying and managing at-risk patients.
We have also recruited eight patient advocates from across south London to support our programmes.
Helping more south Londoners benefit from the latest innovations
Through the MedTech Funding Mandate (MTFM) and Rapid Uptake Products (RUP) programmes, we have had another successful year working with our partners to accelerate the adoption of innovative products designed to improve patient care and health outcomes.
This has meant many more south London residents have benefitted from the latest cutting edge technology and products including a non-invasive procedure for patients with suspected coronary artery disease and an alternative type of medicine for lowering cholesterol.
A key focus for this year has been securing funding for products and long term initiatives which means thousands of more patients are set to benefit over the years ahead.
Key successes have included:
- All Trusts across south London have now adopted MTFM innovations with the majority adopting all eligible products
- 12,000 patients a year have benefitted from new asthma diagnostic devices
- 170 extra patients have benefitted from new severe asthma medicine
- An increase of more than 50 per cent in patients accessing an alternative type of medicine for lowering cholesterol
We have worked closely with partners across south London to deliver the programme, which commenced in 2020. In both acute and primary care, and in all 12 boroughs, providers and commissioners have engaged proactively, helping to get more patients access to effective cholesterol-lowering treatments at the right time.
Helping young people with eating disorders
Since April 2020 we have been working with the whole AHSN Network to support mental health teams deliver First Episode Rapid Early Intervention for Eating Disorders (FREED). This is an innovative service for 16 to 25 year olds enabling them to get rapid and specialised treatment for eating disorders which was developed and piloted by South London and Maudsley NHS Foundation Trust before being adopted nationally.
Good progress continued to be made this year with 74% of eligible Mental Health Trusts now utilising the model. Adoption and implementation will be supported by 38 more FREED Champions who have been recruited to promote early intervention in their service – helping 1000 more young people get the early and tailored support they need.
We continue to work with partners with the aim of ensuring all young people across England have rapid access to treatment by 2023. This will include looking at how we can innovatively support the workforce to deliver this programme in partnership with the FREED Network and NHS England.
Helping people with knee, hip and back pain
ESCAPE-pain is an award-winning programme that helps people with knee, hip and back pain. It stands for Enabling Self-Management and Coping with Arthritic Pain using Exercise and was developed by Professor Mike Hurley at St George’s University of London and Kingston University.
During the last eight years the HIN has worked with partners to introduce ESCAPE-pain to over 300 locations across the UK. This year we were delighted to announce a new partnership with Orthopaedic Research UK who we licensed to run the programme.
Since taking on the license in April 2021, they have supported physiotherapy departments and leisure centres to relaunch the programme. To date, almost 4,000 people have been trained to facilitate ESCAPE-pain and around 20,000 people have attended, saving an estimated £30 million in the costs of health and social care.
Participants frequently report that their pain improves, they take fewer medications and find they are more able to get back to doing the things they enjoy.

Improving outcomes
Learning lessons from Covid-19 to improve mental health services
Covid-19 led to a rapid and almost universal switch to remote consultations in mental health. From summer 2020 we worked closely with partners to understand what this has meant for service users and staff and what lessons can be learned for service models in the future.
This work continued at pace this year culminating in the publication of a comprehensive evaluation report in September which analyses survey responses from 6,000 patients and 700 staff as well as a detailed literature review.
Key findings include:
- Remote service delivery can be acceptable to patients, carers and staff - at least in the short-term.
- Levels of satisfaction may be higher with video calls and that therapeutic alliances may develop more easily in consultations held using video-conferencing software as opposed to telephone.
- There are benefits in terms of convenience in relation to both travel and cost.
Some of the areas to address include computer literacy, privacy and meeting etiquette as well as digital exclusion for some groups and the acceptability of remote consultations for older adults and inpatients. The report also identifies further research needed to fully understand impacts on cost and clinical effectiveness, as well as changes over time.
6000
Patients surveyed
700
Staff surveyed
Equipping clinicians with skills to connect with patients experiencing pain
Psychologically Informed Collaborative Conversations (PIC-C) is an innovative training and supervision course to help health professionals boost their confidence in delivering improved psychologically-informed care for people living with persistent pain.
It was co-designed by people living with pain and in partnership with the Physiotherapy Pain Association, St George’s University Hospital and Kingston Hospitals Chronic Pain and MSK teams.
We worked with partners to pilot PIC-C in 2021 with 38 physiotherapists and published an evaluation of the programme in 2021. All respondents to our evaluation said PIC-C had a positive impact on their confidence in delivering psychologically informed approaches to care.
PIC-C is now available as a commissioned course or as an open course accessed via the Physiotherapy Pain Association.
Improving diabetes care for people with a serious mental illness
People with a serious mental illness are two to three times more likely to have diabetes than the general population. Despite this, Mental Health Trusts do not currently audit inpatient diabetes care.
That is why as co-hosts of the London Physical Health Leads Network, last year the HIN worked with the South London and Maudsley NHS Foundation Trust (SLaM) to pilot an audit on seven inpatient wards, based on the National Diabetes Inpatient Audit. This audit assessed diabetes care in inpatient mental health settings.
Key recommendations from the report include:
- Improving access to diabetes specialists.
- Improving staff and patient education.
- Ensuring policies are communicated and implemented in practice.
- An increased focus on patient centred care.
Following the audit SLaM introduced changes including a diabetes education programme and improved policy communication. The audit template was adjusted and then completed by the other eight London NHS Mental Health Trusts.
The main findings for the London-wide audit identified:
- Eight out of nine Trusts do not have access to their own diabetes specialist resource.
- A need to provide more diabetes education for staff and patients.
- All Trusts need to ensure Trust diabetes policies are implemented in practice.
- Trusts could do more to reduce errors, harms and identify additional health conditions that require medical attention.
- Patient satisfaction was an average of 3.63 out of five, however more can be done to improve patient centred diabetes care.


Harnessing technology to improve treatment for people with long term conditions
Dermatology is one of the services with the biggest backlogs for care caused by Covid-19. With that in mind, since 2020 we have been working with partners to harness the latest technology and innovations to deliver improvements to dermatology services such as streamlining the patient pathway and reducing waiting times.
We supported three dermatology teams, including the two south London ICSs, to redesign their services and implement teledermatology projects. We published a report on these in 2021.
The insights gathered and the case studies produced will help NHS Trusts and commissioners to improve their services and address their dermatology elective care backlog through the use of digital and technological tools. Next year we will deliver phase two to evaluate the impact of these three teledermatology programmes.
Supporting care homes to manage the health of their residents
This year we have worked with South West London Health and Care Partnership and the south east London boroughs to support care home staff to identify when a resident’s health is deteriorating, and take the appropriate action. We have done this by introducing deterioration management tools such as RESTORE2, which are being rolled out nationally.
A wide range of care homes have been supported through this project, including older people’s nursing and residential homes, and homes for people with mental health conditions and learning disabilities.
As a result of this work, 292 care homes across south London are now using deterioration management tools, helping to spot the signs that a resident’s health is deteriorating as early as possible and allowing them to take action quickly.

Ensuring people living with diabetes can access the personalised care they need
Our You & Type 2 programme is designed to make it easier for people living with diabetes to access the care and support they need by combining innovative digital tools with a best practice personalised care and support planning pathway.
Covid-19 meant that people did not always get access to the diabetes care they needed, so last year we worked with partners to trial You & Type 2 @Home. This programme uses remote technologies to monitor people's health and to receive care planning appointments via video or phone at a time when face to face care has been difficult. So far over 100 patients have benefitted from the initiative.
Colleagues working in primary care have experienced exceptional pressures during the pandemic, and to ensure they are able to offer care to those most in need, many practices have used risk stratification tools. This year we have worked with healthcare professionals to embed this approach within You & Type 2, training four new practices in south London to use the pathway. This has helped ensure that people with the greatest need are prioritised for high quality personalised care and support planning.
Developing the skills of care home managers
In 2020/21 we were delighted to continue our partnership with My Home Life England to deliver the Care Home Pioneer programme, a leadership support and professional development programme for care home managers, deputies and senior nurses in south London.
The programme aims to advance skills, facilitate personal growth, and enable our Pioneers to more effectively manage the complex everyday issues that they face as care home leaders.
Due to Covid-19, this year’s cohort of 14 Pioneers attended virtual workshops and action learning sets. They were also introduced to service improvement concepts, with a view to implementing a small quality improvement project within their home.
There will be 36 Pioneers in Cohort 4 and this programme will be delivered over the next year.
Supporting Innovators
Celebrating five years of DigitalHealth.London supporting innovators and the NHS
DigitalHealth.London was launched in 2016 by London’s three Academic Health Science Networks (AHSNs) and MedCity, with additional partnership and funding from CW+ and the Greater London Authority. DigitalHealth.London aimed to transform London into the global capital of digital health by addressing some of the challenges that were holding innovators back.
On top of these programmes, to celebrate DigitalHealth.London’s fifth birthday in October 2021, we started a five-week conversation with NHS and social care staff, the digital health industry, patients and academics to learn lessons from the last five years and identify the best opportunities in digital health over the next five years.
Five key insights from the last five years were identified, including the importance of co-design and building digital capacity. Five key opportunities for the next five years were also established and include joining up systems to allow for digital delivery, the importance of remote digital offers and using data to personalise, predict and empower.
Do you think we should stop calling it “digital health” and instead call it just “health”?
Based on 167 votes across an audience of NHS and social care staff, digital health staff, digital health industry, academics and patients/citizens.
DigitalHealth.London Accelerator and Launchpad programmes
2020/21 saw cohort five welcomed to the DigitalHealth.London Accelerator. The 20 digital health companies, who are tackling significant NHS and social care challenges, were supported for 12 months with bespoke advice, a programme of expert-led workshops and events, and brokering of meaningful connections with NHS organisations.
Cohort six of the Accelerator was announced in January 2022. From apps to AI, remote monitoring to telephony, and mental health to cancer, the solutions from the 21 selected companies are set to transform pathways across the sector. Twenty-four per cent of the sixth cohort identify as being ethnic minority owned, 39 per cent are either female-majority owned or there is no clear majority and 10 per cent are partly or majority owned by a person with a disability.
This year we also announced that nine companies had been selected for the fourth cohort of the DigitalHealth.London Launchpad programme. The three-month programme will support the companies by providing access to knowledge sharing events that will help them understand demand and bring the product or process to market.
143
companies supported through the Accelerator programme in total
90%
of SMEs demonstrated growth whilst on the Accelerator programme
94%
Accelerator success rate (companies still in business)
1498
jobs created
64
new products launched to NHS market
For every £1 spent on the Accelerator through the AHSNs, £12.70 is saved for the NHS
For every £1 of funding spent on delivering the Accelerator, £14.50 is generated into the regional economy
DigitalHealth.London looks to international opportunities
This year we were proud to announce two transatlantic partnerships with two US Accelerators, Cedars-Sinai and MassChallenge.
It means patients in both the UK and US should benefit more quickly from health tech innovations. The partnership will also utilise the deep healthcare knowledge and networks held by both organisations, to support companies who have taken part in the Accelerator programmes, to navigate and gain traction in a new global market and ensure the population of south London benefits from world class innovations.
117
fellows supported across 45 organisations in total
60%
reported a promotion, new job or secondment during the support
55
digital technologies adopted
22%
of projects accelerated their pace of adoption due to the Fellowship
Supporting the next generation of NHS innovators
In October 2021, 37 NHS staff leading digital transformation projects in their organisations completed DigitalHealth.London’s Digital Pioneer Fellowship programme. The Fellows represented a range of NHS disciplines including doctors, nurses, Allied Health Professionals, projects managers and IT staff. The cohort also reflected the NHS workforce, with 30 per cent identifying as being from an ethnic minority and 65 per cent as female.
The projects covered a range of areas. For example, Mark Needham, Programme Director for Digital First, focused on implementing remote monitoring in care homes, while Annie Murphy, a GP at Wide Way Medical Centre, created a GP SatNav. Arron Thind, a doctor at Guy’s and St Thomas’ NHS Foundation Trust, delivered a project pioneering simulation-based medical teaching.
Catalysing local innovation
This year our Innovation Grants programme supported five projects implementing new solutions directly with patients, with the aim of collecting real world evidence and evaluation. The scheme links NHS teams and local boroughs with commercial innovators and guidance from technology experts.
All of the chosen innovations align to key NHS priorities by addressing major health challenges such as managing musculoskeletal pain, mental health and supporting people with long term conditions.
The winning projects included:
- Fun and Fitness – a community sports development programme to support adults with learning disabilities to increase exercise and improve physical and mental health outcomes. The project is run in partnerships between Oxleas NHS Foundation Trust, Royal Borough of Greenwich, Greenwich Leisure Limited and Mencap’s Round the World Challenge.
- Empowering patients with Inflammatory Bowel Disease (IBD) - a pilot project with Kingston Hospital (team members pictured right) where patients with IBD are able to self-manage their care and communications with clinical teams via a digital patient portal known as ‘Zesty’ that is integrated with their electronic patient record.
Each project was given between £10,000 – £30,000 to help them deliver the initial results needed to justify wider-roll out. Many projects are working with local boroughs and a wide range of commercial partners.
Bringing innovators and health care professionals together
We are uniquely placed to bring people and organisations together to develop, test and spread the latest innovations and improve health and care in south London and support elective recovery.
Our Innovation Exchange programme continues to go from strength to strength. This year the Innovation Exchange has organised large-scale events on Transforming Cancer Diagnosis Through Technology and AI and Modernising Primary Care Telephony.
These events convene audiences of over 100 NHS and social care professionals and are an opportunity to put the latest technology in front of those who would benefit most from their spread and adoption.
Together with UCLPartners and Imperial College Health Partners, we also hosted a pan-London Innovation Exchange webinar on Innovations for Cardiovascular Pathways in Community Diagnostic Centres (CDC).
The innovations that were presented at the event were selected based on issues identified through our engagement with stakeholders and focused on cardiology and the pathways linked to heart failure, atrial fibrillation, chest pain and valve disease. Over 100 people registered to hear presentations and pitches from six Innovators specialising in applications for workforce, admin support and cardiovascular-specific innovations.
Along with DigitalHealth.London we also co-produced two round table events on Digital Consent and Digital Pharmacy and e-Prescribing. These small events bring together a curated list of experts from the NHS and industry to discuss the topics with a view to publishing a thought leadership piece.
Evaluating innovation
"The HIN is becoming known for delivering commissioned place-based specialist evaluation and informatics support to health and care organisations in south London and beyond.
We are also increasingly delivering this work for regional and national stakeholders. The HIN can uniquely combine expertise on evaluation and informatics with expertise from its clinical and cross-cutting work programmes and system partners.”
Andrew Walker, Head of Evaluation and Implementation Science
Understanding how micro-volunteering can support health and care
Micro-volunteering is a form of volunteering that comprises of short activities, easily accessed and completed by volunteers in a way that is informal and convenient - usually via digital platforms.
We carried out a wide-ranging evaluation of micro-volunteering models in health and social care on behalf of NHSX and NHS England and completed and published the findings this year.
The evaluation showed micro-volunteering can engage people during a crisis like the pandemic with over 100,000 individuals carrying out over 1.5 million tasks between March/April 2020 and January 2021.
There was good evidence that micro-volunteering works as a way of mobilising a willing volunteer force in meeting unmet community needs and the platforms were good at engaging people who are traditionally less likely to volunteer, particularly those of working age.
83%
found it easy and straightforward to get involved.
96%
found it flexible around the time they gave
79%
felt well supported
82%
felt tasks were a good match for them.
85%
felt they could support their local community
72%
were likely to continue micro-volunteering over the next 12 months
“The potential is enormous as this is a new way of volunteering due to Covid - helping out your neighbour, so this is the right time to capture that spirit and have some infrastructure in place to formalise and modernise the community spirit for the 21st century.”

“The app is a good reminder of what a healthcare professional has said in consultation when there is little time and a lot of information to digest.”
getUBetter user
Helping patients with lower back pain self-manage their condition
The getUBetter app provides digital self-management for individuals with musculoskeletal (MSK) conditions. This year we completed work with partners to scope and evaluate the effectiveness of getUBetter and published the key findings including how easy people found the app to use and the impact it has on the treatment for their condition.
The analysis found that 835 patients were prescribed getUBetter for lower back pain, 50 per cent of whom activated their account. Compared to non-users, getUBetter users required four times fewer GP appointments, 20 per cent fewer physiotherapy referrals and over 50 per cent fewer prescriptions.
Most liked aspects of the app as reported by patients:
- Easy to use
- Helps me develop skills to manage my injury/condition
- Provides relevant information according to my stage of recovery
- It gives me reassurance
In terms of clinicians, 79 per cent reported making referrals to the app and 90 per cent thought that the app supported patients with MSK conditions to self-manage.
Learning lessons from Covid-19 patient care initiatives
To reduce pressures on its acute services caused by Covid-19 in July 2020, Croydon Health Services NHS Trust introduced a virtual ward model to treat acutely unwell patients at home.
Last year we conducted a rapid evaluation into the Croydon virtual ward to understand the impact it had on patients and lessons learned from the implementation.
This found that the model used in Croydon was able to:
- Appropriately deliver care in patients’ homes for 65 per cent of virtual ward patients (all of which were acutely unwell).
- Manage a cohort of up to 30 patients at one time using only a small team of clinicians.
- Provide over 87 per cent of patients with a positive experience when using the virtual ward kit.
Through the model, life limiting conditions were picked up and treated early. The service continues to monitor acutely unwell patients.
43
Facilitated 43 new research collaborations in total
12
Delivered 12 workshops and evidence pitching events
30
Delivered 30 1:1 sessions
£45k
raised in grant funding in total
9
evidence generation webinars delivered with over 1300 registrations and over 600 live participants
Bringing together innovators and academic partners
This year through the DigitalHealth.London Generator we facilitated five collaborations between Accelerator companies and academic partners, bringing the total to 43. A series of four workshops combined with 15 one to ones supported the companies on the fifth cohort of the Accelerator with their evidence generation, from establishing their tier on the NICE Evidence Standards Framework to connecting them with experts.
Following the success of the first #EvaluateDigiHealth series, a second series was launched in March 2021, with the first webinar taking place in April. The DigitalHealth.London Generator once again collaborated with University College London (UCL), the Health Innovation Network (HIN), and MedCity to host a free series of webinars targeted at an international audience of digital health developers, researchers, students, clinicians and NHS managers and commissioners. Topics included experiences of digital health companies in generating evidence, the support available for innovators, perspectives of health care commissioners and staff, regulation for data-driven technologies and evaluation for AI.
Tackling inequalities in health and care
Creating High Volume Low Complexity fast track hubs is a key NHS England programme aimed at reducing the backlog of patients waiting for low complexity operations due to Covid-19 and improving access to care.
As part of work to ensure equity of access to care for all people, in partnership with Imperial College Health Partners (ICHP) we were commissioned by NHS England London to undertake six retrospective Equality Health Inequalities Impact Assessments for the ‘High Volume Low Complexity’ fast track surgical hubs. Together with ICHP we gathered insights from data analysis, stakeholders and patients to review whether protected groups were negatively impacted compared to other surgical pathways. A number of recommendations were provided by the five ICSs to take forward including improved communication with patients whilst they are on waiting lists, more consistent use of interpreters and better planning to meet social care needs.
People and Finance
Promoting diversity in our organisation and work
Two of our values are Different and Together. We are proud to challenge ourselves to stand up to, and go beyond, the AHSN diversity pledges.
At the HIN equality in practice means, for example, that we ensure our engagement programme is co-designed with staff. During Pride month, Black History month and LGBTQ+ history month, we invited external speakers and innovators to share their products and lived experiences. In May 2021 following a ‘lunch and learn’ workshop on menopause offered to all staff we also provided the award-winning ‘Peppy Health’ menopause support licences to all those who wanted them.
We continue to progress our work on our ambition to be an actively anti-racist organisation. In December 2021 the Board approved our proposals to deliver on this ambition. This followed a series of organisation-wide conversations in 2020/21 in response to the George Floyd murder, after which we committed to taking action around racial inequalities and inequity through our work, and in our workplace. Several concrete steps have now been taken to develop an organisational approach to anti-racism:
a) We have raised awareness of the impact of racism - on our staff, organisation, and health outcomes of the population we serve by holding a series of conversations with staff where we gathered a range of insights.
b) We have appointed an external expert in the anti-racism field to advise and support us to create a culture that is psychologically safe enough to speak up and challenge racism and introduce meaningful change within the organisation – through the way we are with each other and the work we do in south London and beyond.
c) We have established a thriving ‘Reducing Health Inequalities’ community of practice which has created a space for staff to learn, share, collaborate and find creative solutions to how we can tackle health inequalities through our work.
The HIN's ambition for anti-racism:
Leadership
Anti-racism is led from the front and the HIN is recognised as a leader in antiracism in the system
Action
Our words are followed by meaningful actions, operational and structural commitments and transparent measurement
Culture
Collectively, we champion antiracism, support psychological safety and create a learning environment founded on humility, curiosity and accountability
Health inequalities
We are knowledgeable and comfortable talking about racial inequity, racism and therefore able to contribute to addressing health inequalities as part of our work
Speaking up
We have the confidence, language and tools to speak up and challenge and encourage others to do so kindly and productively
Positive experience
Regardless of ethnicity and background, staff feel heard, valued and supported to contribute to major organisation activities
Recognition and understanding
As individuals and a community, we know and feel why this is important (we take steps to educate ourselves, show empathy and take responsibility for our actions)
Finance tables
- Expenditure
- £’000
- PayNon-PayTotal
- Central Costs
-
7798221,601
- Corporate Support
-
565-565
- Communications
-
37692468
- CVD Prevention
-
1350135
- Diabetes
-
26713281
- Patient Safety & Experience
-
65697752
- Healthy Ageing
-
280135415
- Mental Health
-
203104307
- MSK
-
241104345
- Innovation
-
376131507
- Graduates into Health
-
418271689
- Technology
-
2852287
- Insight
-
53938577
- Digital Health.London Accelerator
-
710172881
- Total
-
5,8301,9817,811
- Income
- £’000
- Core Income
- 4,205
- Membership
- 465
- Other NHS
- 1,406
- Universities
- 58
- Third Sector
- 175
- Escape Pain
- 11
- Graduates into Health
- 532
- ERDF
- 480
- Industry
- 117
- Techforce
- 519
- Total
- 7,448
Pay gap
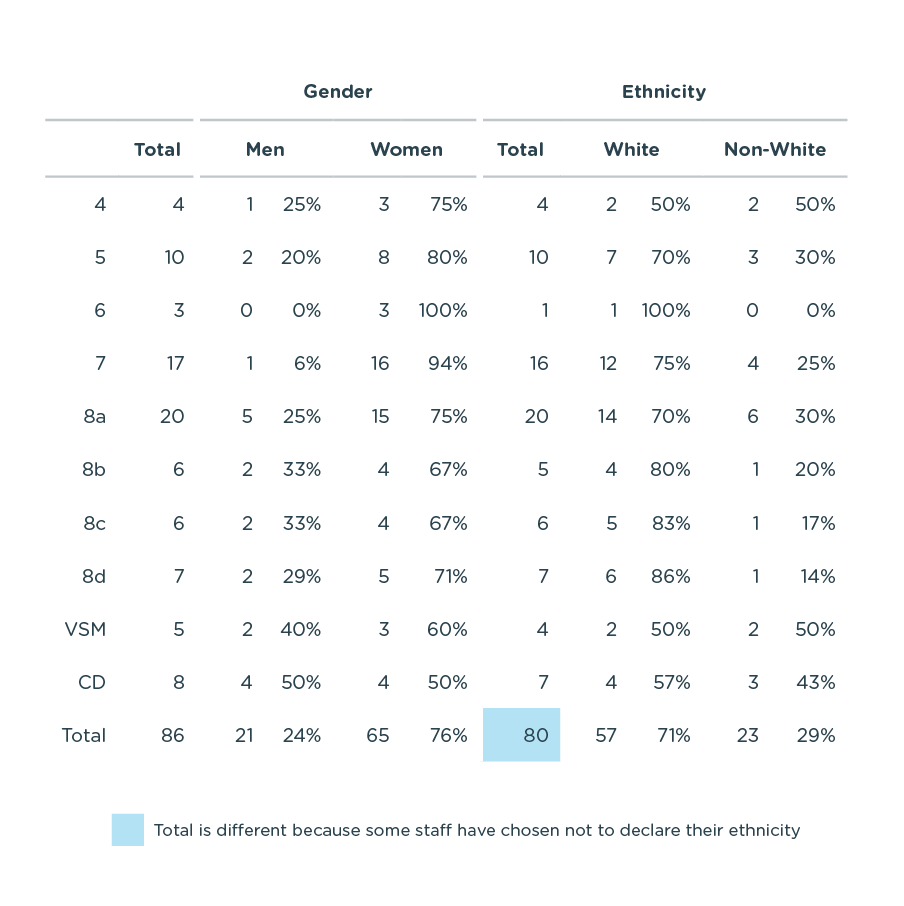
Here at the HIN we are committed to improving diversity, inclusion and equality. That is why, in the interests of transparency, we have published data related to staff gender and ethnicity pay gaps on an annual basis for several years. The latest available data for 2021/22 is published below.
As the HIN is relatively small organisation, caution should be exercised when interpreting the data, particularly where the dataset is further broken down, for example where colleagues are separated into particular pay grades.
Nevertheless, we recognise that as a staff group we do not fully represent the diversity of the south London population that we serve, which is why we are working to avoid bias in our recruitment and ensure that the HIN is an inclusive and welcoming employer, including our ongoing anti-racism work. Externally we continue to work hard to involve people at highest risk of experiencing health inequalities in all our projects and encourage our partners to do the same.
Gender
Mean hourly pay: men 27 per cent higher than women. In 2020/21, the mean hourly rate for men was 20 per cent higher than women.
Median hourly pay: men 14 per cent higher than women. In 2020/21, the median hourly rate for men was 31 per cent higher than women.
Ethnicity
Mean hourly pay: those who identify as being from an ethnic minority 7 per cent higher than those who identify as white. In 2020/21, the mean hourly rate for people who identify as white was 2 per cent higher than people who identify as being from an ethnic minority.
Median hourly pay: those who identify as white 11 per cent higher than those who identify as being from an ethnic minority. In 2020/21, the median hourly rate for people who identify as white was 14 per cent higher than people who identify as being from an ethnic minority.
It is worth noting that this is driven by salaries across a range of staff roles and working patterns.
Breakdown of Diversity by band