People who are particularly vulnerable or isolated as a result of the coronavirus (Covid-19) outbreak could soon benefit from a range of innovative digital solutions selected as part of the TechForce19 challenge.
NHSX and MHCLG have announced 18 digital solutions that have been awarded funding under the TechForce19 challenge. TechForce19 has awarded up to £25,000 each to innovation that offers a digital way to support vulnerable people who need to stay at home or need other help in the community for extended periods of time. The response to the challenge was extremely strong, with over 1,600 innovations submitted.
The successful solutions will now receive funding to rapidly test their product to meet specific Covid-19 related needs.
This testing phase will last for two to three weeks, and be followed by an assessment to better understand the potential and scope for accelerated deployment at scale, based on evidence.
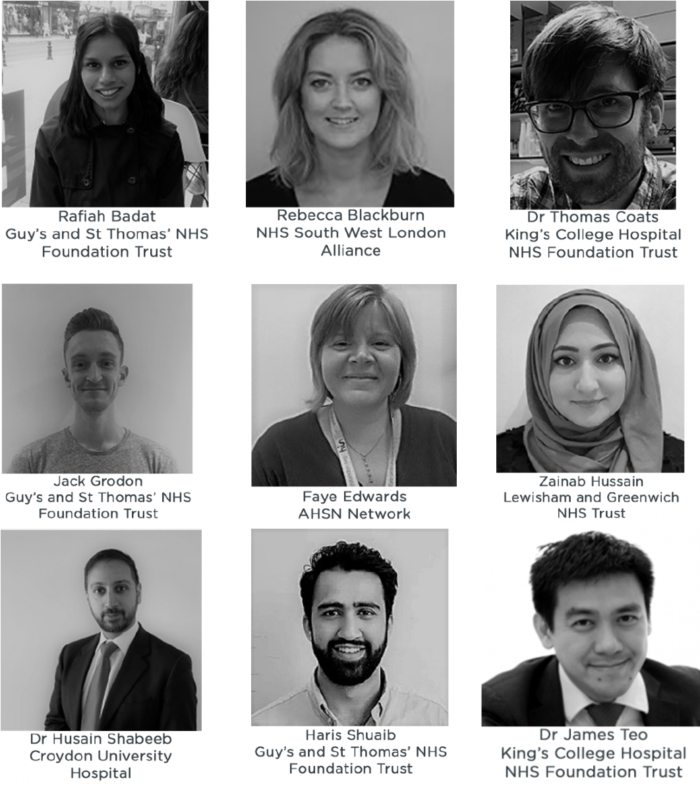
NHSX has been working with partners PUBLIC and the AHSN Network to run the fast-track competition for innovators, creating a pool of technologies that have the potential to be rapidly scaled regionally and nationally.
Each prospective technology must have the capability to operate on a standalone basis without the need to be integrated with existing health or care systems.
Examples of the solutions going forward include:
- Feebris for the most vulnerable who are isolating
Feebris helps carers to identify health risks and deterioration within elderly communities. The Feebris app guides a carer through a 10min check-up, including capture of vital signs from connected medical-grade sensors (digital stethoscope, pulse oximeter etc.). Powerful AI augments clinical guidelines and personalised monitoring to help decisions on triaging health issues. The intention is to provide Feebris to care homes to help carers triage the day-to-day health needs of their residents during the Covid-19 pandemic, and also enhance the capabilities of remote clinicians.
- Neurolove to support young people with mental health
Chanua provides Neurolove.org, a platform providing a friendly ear and human support for young people to help them to keep virtually social and safe online. Supporting young people to manage anxiety and low mood, they can book sessions directly with mentors and therapists and find content that will support them to manage their emotional and mental health in this current period of uncertainty.
Peppy helps parents-to-be and new parents remotely access trusted, convenient advice from perinatal and mental health experts. This includes remote support via phone/video with lactation consultants, baby sleep consultants, specialist mental health support and more. Peppy provides timely interventions that reduce stress, anxiety and burn out for parents-to-be and new parents.
- Team Kinetic for volunteers
TeamKinetic’s digital platform helps organisations better manage community-led volunteer programmes. The solution helps manage recruitment and retention of volunteers, as well as monitoring the impact of these programmes in real time. TeamKinetic are also looking at developing and documenting some open standards and establishing a model for better service interconnectivity across the voluntary sector.
- Vinehealth for cancer patients
Vinehealth is a mobile app to support cancer patients and their loved ones during treatment by allowing them to easily track and understand their care, including their symptoms, side effects, appointments and medications. By completing a 1-minute daily log, cancer patients can develop a clear overview of their progress through treatment and access advice on how to cope and when to access health services. The Vinehealth app empowers cancer patients who are self-isolating to self-manage and feel more in control.
“The TechForce19 challenge has harnessed some of the incredible talent we have in our tech sector to help the most vulnerable. Many of the problems created by isolation lend themselves to digital solutions, and we hope this process will help people take advantage of the potential that digital technology offers.
“The 18 companies we are announcing today have the potential to help a number of the key affected groups during Covid-19, including young parents, the elderly at home, and the homeless, as well as giving people tools to look after their own mental health during isolation.”
Guy Boersma, Digital & AI Lead, The AHSN Network, said:
“This list of solutions is testament to the talent being harnessed to address the consequences of the Covid-19 crisis. The health and care sector has already seen many solutions being deployed to support vulnerable citizens with mental health needs or other specific conditions, and the pandemic makes it even more necessary that we address the needs of citizens unable to access face-to-face care or even their usual social networks.
We are delighted that we have a series of solutions which can be piloted and then scaled to address these pressing needs.”
Daniel Korski, CEO of PUBLIC, said:
“As social distancing measures continue, today’s selections amount to a wealth of possible answers to helping the most vulnerable through these difficult times.
These companies demonstrate the valuable role for new technologies in helping public services adapt to new challenges, and we’re excited to follow their journeys from here through to deployment.”
For more information about the programme visit Techforce19.uk
Full list of digital innovations:
- Feebris for the most vulnerable who are isolating
Feebris helps carers to identify health risks and deterioration within elderly communities. The Feebris app guides a carer through a 10min check-up, including capture of vital signs from connected medical-grade sensors (digital stethoscope, pulse oximeter etc.). Powerful AI augments clinical guidelines and personalised monitoring to help decisions on triaging health issues. The intention is to provide Feebris to care homes to help carers triage the day-to-day health needs of their residents during the Covid-19 pandemic, and also enhance the capabilities of remote clinicians.
- Chanua / Neurolove to support young people with mental health
Chanua provides Neurolove.org, a platform providing a friendly ear and human support for young people to help them to keep virtually social and safe online. Supporting young people to manage anxiety and low mood, they can book sessions directly with mentors and therapists and find content that will support them to manage their emotional and mental health in this current period of uncertainty.
- Peppy for new parents
Peppy helps parents-to-be and new parents remotely access trusted, convenient advice from perinatal and mental health experts. This includes remote support via phone/video with lactation consultants, baby sleep consultants, specialist mental health support and more. Peppy provides timely interventions that reduce stress, anxiety and burn out for parents-to-be and new parents.
- Team Kinetic for volunteers
TeamKinetic’s digital platform helps organisations better manage community-led volunteer programmes. The solution helps manage recruitment and retention of volunteers, as well as monitoring the impact of these programmes in real time. TeamKinetic are also looking at developing and documenting some open standards and establishing a model for better service interconnectivity across the voluntary sector.
- Vine Health for cancer patients
Vinehealth is a mobile app to support cancer patients and their loved ones during treatment by allowing them to easily track and understand their care, including their symptoms, side effects, appointments and medications. By completing a 1-minute daily log, cancer patients can develop a clear overview of their progress through treatment and access advice on how to cope and when to access health services. The Vinehealth app empowers cancer patients who are self-isolating to self-manage and feel more in control.
- Beam for homeless population
Beam is a digital platform that supports the homeless and vulnerable people sleeping rough. Beam takes referrals from local authorities and homeless charities, then ensures goods are funded, delivered and documented.
- Alcuris Ltd
Alcuris’ Memohub® prolongs the independence of elderly or vulnerable people, enabling them to return to home quicker, from hospital discharge. A digital platform collates data from unobtrusive sensors placed in the home, then provides actionable alerts when behaviour changes, enabling families to intervene early to delay or reduce the frequency of professional ‘crisis intervention’ help. This gives family a reassurance of loved one’s safety and wellbeing even when left alone for extended periods. Also provides objective information to inform professional care planning.
- Ampersand
Ampersand Health‘s self-management apps help people with long term, immune mediated diseases (such as Crohn’s and Colitis) live happier and healthier lives. Using behavioural and data science, the apps deliver courses and programmes designed to improve sleep quality, stress management and medication adherence; with modules for activity, diet and relationships in the works. During the Covid-19 crisis, this will help these people better manage their conditions and reduce the need for clinical support. Ampersand are also offering their clinical management portal free of charge to NHS Trusts until January 2021, no strings attached. This will allow clinical teams to help manage their patients, remotely.
- Aparito
Aparito uses remote monitoring technology (videos, wearables, photos and text) to gather patient-generated data outside of hospital. This is focused on patients with rare diseases. Data is captured and transferred via the patient’s own smartphone / tablet and made available to clinicians or researchers in real-time to help avoid direct contact during the Covid-19 crisis.
- Birdie
Birdie provides a digital platform for home care agencies to better manage the care they provide. Through an easy to use app, care workers capture daily visit logs, and a central hub allows staff to track real-time information. Family members receive live and daily safety and well-being updates through the app, including from optional home monitoring sensors. Birdie helps domiciliary care agencies to increase efficiency, and improves the care people receive in their homes through systematic monitoring, prevention of risks, and support to carers.
- Buddi
Buddi Connect is a smartphone app, enabling people to stay in touch with those they care for. Safe groups of connections are united through the app to share private, secure messages and raise instant alerts when help is needed. Important messages from the NHS can be shared directly to users. During this difficult time, while many vulnerable people are missing the face-to-face contact of family, friends and carers, the reassurance that help is available at the touch of a button is more important than ever.
- Just Checking
Just Checking supplies activity monitoring systems, used by local authorities to help with assessment of older people in their homes, for social care. Sensors pick up activities of daily living and display the data in a 24-hour chart. The company also has a second, more sophisticated activity monitoring system, to help manage the care and support of adults with learning disabilities.
- Peopletoo Ltd/ Novoville
Peopletoo and Novoville have been selected to launch GetVolunteering, a volunteering app to fast track volunteers into clinical and non-clinical roles to support the fight against Covid-19. It will enable local authorities to quickly identify and assess capable volunteers in the local community to fill key roles to support social care in areas that have been impacted by loss of staffing capacity due to Covid-19, or for new roles that are required during the crisis.
- RIX Research & Media, University of East London
The RIX Multi Me toolkit provides highly accessible and secure social networking that serves as a support network for people with learning disabilities and mental health challenges. This easy to use multimedia network, with accompanying communication, personal-organiser and goal-setting tools, enables isolated and distanced vulnerable people to build stronger support circles. It helps them self-manage their care and actively limit the impact and spread of Covid-19 infection. Care professionals use the ‘Stay Connected’ RIX Multi Me Toolkit to remotely monitor and support people’s wellbeing in an efficient and friendly way.
- Simply Do
Simply Do will develop a virtual community of NHS medical professionals currently in self-isolation. These employees have significant expertise, experience and skills which can be unlocked virtually to help solve Covid-19 care challenges set within the platform. This will create a powerful ‘think-tank’ of medical professionals to contribute virtually to fight Covid-19 by solving wider health challenges (i.e. challenges faced in the care sector).
- SureCert
SureCert is a digital platform that connects people with job and volunteering opportunities. The system also manages background checks. SureCert can provide data on successful placements, and information to enable policy makers to better understand the labour market and volunteering supply and demand.
- VideoVisit Global Ltd
VideoVisit® HOME allows the elderly to communicate with their family members and home care providers through a virtual care tablet designed specifically for elderly. VideoVisit will measure how this virtual home care service can increase people’s feeling of safety and decrease loneliness during self-isolation.
- Virti
Virti aims to make experiential education affordable and accessible for everyone. Virtual and augmented reality, coupled with AI, transports users into difficult to access environments and safely assesses them under pressure to improve their performance. The system is used for training and patient education.