Protected: Reducing access inequalities to proven lipid treatments in Bexley


One in every two people in England will be diagnosed with cancer at some point in their lives. Medical innovation has driven huge improvements in cancer outcomes; thanks to advances in treatments, diagnostic techniques and screening, survival rates have doubled in the past 50 years. However, with a growing and aging population, using innovation to detect cancers earlier and ensuring treatment is as effective as possible, remains an important point of focus for the NHS.
In England, many of the system’s cancer priorities were set out in the NHS Long Term Plan in 2019. These include:
In south east London, additional priorities can include improving processes and efficiency in cancer data and pathway management to enable smarter work flows. Or, improving the early identification of cancers through screening and diagnostics, with a particular focus on individuals at risk of health inequalities such as people from more deprived areas.
As with many areas of health and care, the cancer system has grown to be highly complex, with many interdependencies and interfaces between radiology, pathology and across other services.
In particular, the timely treatment of suspected cancer cases often rests on effective coordination between primary and secondary care –which requires appropriate and timely referrals. This then followed through with an effective booking and triaging once to manage patient flow and ensure the patient receives the correct treatment.
Used effectively, technology offers the promise of reducing some of the complexity associated with managing cancer pathways and improving both staff and patient experience. Broadly speaking, many digital innovations which seem to offer the most benefits can be grouped into two categories:
Many recent digital innovations are already seeking to make an impact to cancer pathways; some examples include:
With clear targets for cancer performance at both national and regional levels, successful innovations need to be able to demonstrate tangible impact in one or more key performance indicators. Other important considerations for successful spread and adoption include ease of implementation/integration and patient and staff experience.
The Health Innovation Network South London has extensive experience supporting innovations across a wider range of clinical areas, including cancer. Through our DigitalHealth.London programmes, we have worked with some of the capital’s most promising cancer tech companies, helping great ideas to achieve real-world impact.
We also work with systems and services to evaluate, understand and implement cancer innovations. With the speed of progress in many areas of digital innovation, such as AI being extremely high and a workforce busy with operational pressures, we can provide specialist support to identify innovation opportunities and overcome challenges to make the most of technology. We have recently collaborated with the South East London Cancer Alliance (SELCA) and its clinical and cancer management networks on a number of innovation areas including exploring the opportunities of automation, needs articulation, horizon scanning and supporting the evaluation of local innovation projects.
“It’s been fantastic to work in collaboration with the HIN to identify potential digital solutions for challenges faced by cancer services. Our expertise in cancer pathway improvement combined with the HIN’s experience of embedding digital innovations across the NHS, will help us to explore innovative ways to transform our local cancer care services and improve patient experiences.”
Smitha Nathan, Associate Director, South East London Cancer Alliance
Get in touch with our team to find out how we’re supporting better outcomes and more efficient services.
Email usThe Health Innovation Network (HIN) South London has been running the flagship Graduates into Health programme since 2018. Over the past six years the programme has recruited graduates and early careers professionals from across the UK and internationally to fill digital, data and technology roles throughout England.
The programme, funded by NHS England, closed on 31 March 2024. In this co-authored blog we hear from Head of Service Louise Brennan, Engagement Lead Project Manager Karniya Yoganathan and Pastoral Support Lead Charlotte Gallagher as they reflect on the successes of the programme sourcing new talent to drive innovation in healthcare.
In my position as the Head of Service for the Graduates into Health programme, I’ve led a journey of significant transformation over the past six years. Our main aim has been to pioneer a programme that not only meets the growing digital needs of the NHS but also nurtures fresh talent to drive innovation in healthcare.
Our journey began in 2018 with a vision to bridge the gap between the increasing demand for digital skills in healthcare and the availability of skilled professionals within the NHS. Starting at a local level, we worked to expand our initiative into a national programme, supporting over 240 graduates in securing vital roles in Digital, Data, and Technology (DDaT) within the NHS.
One of my proudest achievements has been the establishment of the first-ever graduate DDaT programme within the NHS. Prior to this, similar programmes were either found in the private sector or delivered fast-track graduates into leadership positions. Recognising the crucial need for digital expertise in middle-management public healthcare, we embarked on a mission to fill this gap.
Our programme not only addressed a critical need but also gained support from NHS managers seeking to enhance their teams with fresh talent. Through careful recruitment and rigorous training, our graduates demonstrated their skills, earning praise for their proficiency and adaptability. This success led to repeat requests from managers, solidifying our programme’s reputation as a valuable asset to NHS organisations across the country.
Our expansion from London to regions nationwide highlights the scalability and impact of our initiative. By aligning with key NHS priorities around digital transformation and workforce planning, such as the NHS Long Term Workforce Plan, we’ve contributed to modernising healthcare delivery and improving patient outcomes.
Ultimately, the impact of our programme is seen in the tangible improvements observed in organisations undergoing digital transformation. By empowering a new generation of digital graduates, we’ve not only addressed immediate workforce needs but also laid the groundwork for a more resilient and innovative NHS ready to meet the evolving challenges of healthcare delivery in the digital age.
“We often struggled to get suitable candidates and so a typical recruitment would take far longer than 6-8 weeks because we’d have to go out again and again. We recruited for one position through the Graduates into Health programme and were so impressed with the quality of the candidates that we ended up taking two!”NHS Informatics Merseyside Software Developer Manager
Working as the Engagement Lead Project Manager for the Graduates into Health programme, I supported the overall programme delivery and oversaw tasks including trust engagement, pastoral care and mentorship activities. As the programme nears its end, I take pride in reflecting on our achievements.
A significant aspect of our success lies in our ability to achieve diversity and retention goals. The Graduates into Health programme has prioritised inclusivity, with 57 per cent of participants coming from ethnic minority backgrounds and 44 per cent identifying as female. This commitment to diversity has contributed to our impressive 91 per cent retention rate, showing that the programme effectively supports career advancement within the NHS.
One notable accomplishment is our contribution to bridging the NHS’s skills gap which was particularly evident in our efforts in to recruit in rural areas. An example of this was our successful recruitment of twelve Band 6 configuration analyst graduates to contribute their skills to the implementation of North Devon Health Care Trust’s ‘My Care’ Epic Electronic Patient Record Programme. Positive feedback from these placements highlights the effectiveness of our thorough recruitment processes, which assessed graduates’ technical abilities through various tests.
I take great pride in the gender diversity of our programme participants. By empowering women from diverse backgrounds, including those returning to work, the Graduates into Health programme aligns with the NHS’s commitment to fostering an inclusive and gender-equal workforce. This diversity enriches the healthcare sector by bringing different perspectives and skills to the table, ultimately improving patient-centred care delivery.
As we near the end of this programme, I want to express how the Graduates into Health programme has not only provided valuable career opportunities for graduates but has also addressed important skill shortages and diversity issues within the NHS.
In my position I had the privilege of providing individual pastoral support to 130 graduates over the past year as they transition into DDaT roles within the NHS. Our focus has been on providing tailored support to help these individuals navigate the complexities of starting their careers in healthcare.
Central to my responsibilities has been offering personalised guidance to graduates, particularly concerning their well-being and professional development. Through regular conversations, I’ve witnessed their progress and celebrated their achievements as they overcome challenges and take steps forward in their careers.
Embracing a graduate-centred approach, I’ve actively sought feedback from graduates, leading to the implementation of various support mechanisms such as newsletters and networking events. The aim was to keep graduates informed about opportunities within the NHS and foster a sense of community among them.
Feedback from graduates highlights the significance of our support in helping them secure positions within the NHS, even in the face of competition from the private sector. My role has also involved identifying and addressing individual barriers to career advancement, whether they be related to training, working within the NHS, or personal well-being.
As the Graduates into Health programme draws to a close, I’m gratified by the impact our efforts have had in nurturing the talents of these graduates and contributing to the strength of the healthcare workforce. It’s been a fulfilling journey, and I’m thankful for the opportunity to have played a part in their growth and success.
Find out more on the Graduates into Health programme’s success below.
The Health Innovation Network (HIN) South London is launching its third Cardiometabolic Fellowship (formerly Cardiovascular Disease (CVD) Prevention Fellowship). The programme will now assist primary care clinicians develop clinical skills and knowledge in diabetes and mental health care along with cardiovascular disease prevention to help improve outcomes for patients across south London.
Applications to this Fellowship have now closed.
With six million people living with CVD in England with a combined cost of £16 billion every year, improving outcomes for at risk patients is an NHS priority. This programme will help to speed up the adoption of innovative initiatives to help prevent CVD across south London.
This free programme builds on our last two successful Fellowships and is aimed at all health care professionals working in primary care or community pharmacy in south London. The Fellowship aligns to local priorities and supports practices and primary care networks (PCNs) in meeting their Quality and Outcomes Framework targets, reducing health inequalities, and reducing risk to your patients.
“I appreciate the support and guidance I have received throughout the fellowship. Being a part of this program has been an enriching experience, and I am grateful for the opportunity to contribute to improving care for the CVD patient population.”Participant from 2023 CVD Prevention Fellowship.
The Fellowship Programme is Continuing Professional Development (CPD) accredited and will provide free expert clinical advice and quality improvement support to help Fellows become CVD prevention, mental health and diabetes care champions. It will also help Fellows to deliver a quality improvement project focused on CVD or diabetes in their practice or PCN. You can see examples of 2023 projects here.
Running from April 2024 to November 2024, the Fellowship will consist of:
For more information on the Cardiometabolic Fellowship please get in touch.
Contact usResults from a new report from the Health Innovation Network (HIN) South London and NHS England (London) Digital First team indicate that up to three quarters of Londoners have used online consultation forms, the NHS App and GP surgery websites to access primary care services.
More than 3,000 patients from across London contributed to the report by completing an online survey or participating in focus groups. The report indicated that most people found these digital tools beneficial as they allowed them to complete key tasks related to managing their healthcare more independently.
Whilst most patients who responded found the three digital tools easy and convenient to use, the report also highlighted variation across London, with some patients reporting challenges with accessibility and availability of certain features. For example, 43% were not able to book a routine GP appointment online and almost a third did not have full access to their medical records via the NHS App.
The report also highlighted the importance of continuing to tackle the root causes of digital exclusion, acknowledging that some groups underserved by digital technologies may still be underrepresented in this type of research.
Usage of key digital tools
The most used digital tool was the NHS App, which had been used by 87% of people who completed the survey. Generally, patients felt the NHS App was a useful source of information and they valued the ability to manage their own health through ordering repeat medication and accessing their health records.
77% of those surveyed had used online forms to provide information about a health concern or condition to their GP. Patients highlighted that these forms often saved travel and waiting times, although a third of patients found that online forms were not always available for them to use and some reported challenges with lengthy forms to complete.
76% of patients who contributed to the report had used a GP surgery website in the past. Most people felt that GP websites were useful for signposting to self-care and information on how to access GP services. According to some patients, the quality of GP websites had improved; however difficulties remained for others around navigation, requesting routine appointments, and out-of-date information being displayed on GP websites.
Recommendations for improvement
The report also details a number of priority areas for improving the adoption and user experience of digital tools in primary care. It includes suggestions for improvements based on feedback from the patients that completed the survey and attended the focus group discussions, as well as learning and best practice from areas across London.
The recommendations include improved communication with patients about the digital tools available in primary care, driving higher standards of usability and accessibility across the sector, and taking a user-centred approach to engaging patients in service design and delivery. Based on patient feedback, the report also recommends that GP practices consider increasing the amount of time that online forms are available for patients to complete and that they explore enabling more online appointments for patients to book directly. Other suggestions included building in mechanisms to capture timely feedback from patients and making all repeat medications in the NHS App available to order.
Additionally, the report covers a number of considerations related to digital exclusion, identifying the need for flexibility within the use of digital tools to allow for compliance with the Accessible Information Standard where patients have different communication needs.
Discussing the launch of the report, Matt Nye, Director of Digital First Programme, NHS England (London) said:
“This report has shown us how integral digital tools are for people using primary care services across London.
We’ve heard that patients find the most common digital tools really helpful for accessing support in ways that suit their needs, and this provides more evidence for continuing to invest in making these channels as good as they can be.
Optimising digital channels can often provide long-term efficiency savings for practices while improving patient choice. If we can save admin time for busy GP teams through increasing the use of digital tools where appropriate, that in turn frees up time to help people who need to use other routes to access advice or support.”
Amanda Begley, Director of Digital Transformation at the HIN South London said:
“It is great to now have such a rich picture about what is and isn’t working for patients when it comes to digital primary care. With the report identifying high usage rates of the NHS App, online consultation forms and GP websites, making some relatively small improvements as identified in the report could have a big benefit for patients and primary care services.
We also need to make sure digital exclusion remains at the top of the agenda and that primary care teams get the support they need to give patients access to a full range of digital and non-digital options for how they manage their health.”
Aurora Todisco and Faith Smith, Lived Experience Partners at the HIN South London said:
“We are proud that we have involved such a diverse group of Londoners in this project to understand the role that digital tools play in managing some key elements of their health.
Many of the patients we spoke to in our focus groups were really enthusiastic about digital technology, including those from potentially marginalised or digitally excluded groups.
Continuing to work closely with a true cross-section of society will be key if we want to pave the way for solutions which work for everyone.
We look forward to seeing the positive impact that this work will have for people and communities across the capital.”
Please get in touch for more information on our work to understand patient perspectives on digital tools in primary care.
Get in touch
Darzi Fellow Dr Ella Caine writes about her experiences on the programme, how she used the opportunity to shine a light on health inequalities, focusing on the provision of interpreting services in South West London maternity services, and makes her recommendations to support ongoing work.
Having worked as a midwife for nearly 24 years, alongside helping to educate the next generation as a lecturer at the University of East Anglia, I was on the lookout for a new challenge when the opportunity arose to participate in the Darzi Fellowship.
The Fellowship, which is sponsored by South West London Integrated Care System (ICS) and the Health Innovation Network (HIN) South London, involves studying for a postgraduate certificate in healthcare leadership while addressing a challenge in maternal health inequalities. The challenge I chose to address was provision of interpretation services for women and birthing people who do not speak English.
This group experiences significant differences in health outcomes in the UK compared to English speakers. Furthermore, a language barrier can increase misunderstanding and even fear during what can already an intense and life-changing period. Within this group there are further challenges experienced by members of refugee and asylum seeker communities, who not only face language barriers but have often had traumatic prior experiences. My aim was to shine a light on the difference in provision between the four South West London Trusts and beyond, highlighting best practice and suggesting improvements.
Even for native English speakers, navigating NHS maternity services and labour can be confusing. While efforts had been made to improve alternate language provision, it is predominantly available by telephone and online, and is often problematic during emergencies or unexpected situations.
My first few months were dedicated to immersing myself in the four maternity services in South West London, which each provide care in the births of over 3,000 babies per year. There are also significant differences in demographics and wider contexts between the trusts, and my first challenge was familiarising myself with the South West London landscape, as well as identifying and engaging with key stakeholders.
Another important challenge was engaging with the women and birthing people who used maternity services whilst speaking little or no English. To do this I collaborated with third-sector organisations and community groups to reach them through trusted and established channels. It was not always clear in advance who would turn up to sessions, so I had to remain flexible. I also took the ethics of my research very seriously. Sponsorship by the HIN and South West London ICB ensured fair reimbursement for participation, obtaining consent and engaging with participants in an open, honest and transparent way. Overall. I felt very privileged to be welcomed into these spaces and to be trusted by these communities.
While it was challenging to work on the project in an unfamiliar part of the country while studying at the same time, after an intense year I was able to provide a comprehensive summary of the support available and make a series of recommendations.
While all trusts used phone-based translation services through Language Line, some also employ video interpreters, which added a more relational touch. However, not all interpreters understood maternity care and its terminology, leading to gaps in understanding, and some women and birthing people using the services felt uncomfortable with male interpreters during their care.
There are new innovations available, such as CardMedic, which consists of virtual cards with common questions to aid communication between staff and people accessing maternity services. CardMedic is in the pipeline for some London Trusts, once funding progresses, and is being trialled by another London maternity service.
Beyond London's borders, I encountered Trusts that offered multilingual doulas who stayed on hand throughout labour, offering emotional and linguistic support. In my opinion, this is the most comprehensive level of support available in labour, though it is resource-intensive. This initiative was offered through a voluntary sector organisation and anecdotally led to high levels of women’s satisfaction.
Where possible aim for continuity of interpreter to allow trusted relationships to grow
Care pathways must be amended to include the interpreter as a member of the muti-disciplinary team
Building on this work South West London Local Maternity and Neonatal System (LMNS) should benchmark interpreting services and ensure there is no unwarranted variation across the system
Training and guidelines for maternity and neonatal teams should be provided, benchmarking against the Maternity pan-London guidance (pending publication September 2023)
Development of interpreting services must be coproduced with collaboration between:
a) Women and birthing people
b) Maternity and Neonatal care providers
c) Community assets
d) Maternity and Neonatal Voice Partnerships
e) Maternity core connectors/community engagement practitioners
It was a difficult but immensely rewarding journey, and I am pleased to have participated in serious engagement already on how to address the problems outlined and improve services. Maternal health inequalities, though deeply ingrained, are not insurmountable. By working together to highlight and tackle inequalities when we find them, we can bridge the gap and ensure that everyone, regardless of background, receives the support they need and deserve.
For more information on how we address health inequalities, please get in touch.
Contact usThe Health Innovation Network (HIN) South London and South East London Integrated Care Board (SEL ICB) have partnered to continue work targeting atrial fibrillation by identifying patients who could benefit from life-saving anti-coagulation treatment.
Atrial fibrillation (AF) is a cardiac condition which causes an irregular heart rate and can decrease the efficiency and effectiveness of the heart. This year the HIN and the South East London Integrated Care Board (SEL ICB) have partnered on targeting AF, to continue the work started with the AF Toolkit Programme, in order to improve the pathway that treatment is being delivered.
Rachel Howatson, Senior Cardiovascular Pharmacist at SEL ICB said ‘the benefits of collaborative working between the HIN and SEL ICB are being experienced by many patients and healthcare professionals across the South East London Integrated Care System and we really are making every contact count.’
Direct oral anti-coagulants (DOACs) reduce the likelihood of patients with AF having a stroke. Following NICE guidance, DOACs are considered both safe and effective for the treatment of AF and stroke prevention compared with warfarin which was the conventional treatment option. NHS England (NHSE) now recommends that DOACs are first line treatment for anticoagulation of AF. NHSE estimate that 21,700 strokes could be prevented, and 5,400 lives saved over the next three years thanks to these developments. Through new programmes to expand access to DOACs, NHSE have established agreements which have led to a cost saving per patient.
Cardiovascular Disease (CVD) causes a quarter of all deaths in the UK and is the largest contributor to premature mortality in the deprived areas. The NHS Long Term Plan aims to reduce 150,000 cardiovascular events over the next decade of which Atrial Fibrillation is one of the national priorities. The aspiration is to identify 85 per cent of AF cases and improve anticoagulation rates to 90 per cent by the year 2029. People with AF are five times more like to have a stroke, and the British Heart Foundation estimates that 270,000 people aged over 65 are living with undiagnosed AF.
SEL ICS redesigned clinical pathways to ensure more patients have access to the latest treatment according to national and local guidance. The HIN supported the SEL ICS through project management to deliver an AF detection programme. This supports the national aims to increase the detection of AF and we have utilised resources to re-invest in AF detection to identify patients who may benefit from anticoagulation.
Creating clear guidance has been important in terms of the raising awareness of detection of atrial fibrillation as well as its management and ensuring that processes are not prohibitive to the care of patients. This programme is aimed at detecting undiagnosed AF by deploying non-invasive devices that can quickly and accurately detect an irregular heart rate. Patients can then be referred for investigations and treatment. This allows patients to access potentially lifesaving anti-coagulation and reduce their risk of having a stroke.
This project highlights the importance of clinicians and colleagues working towards the NHS Long term plan of reducing 150,000 CVD events over the next decade. The early diagnosis and treatment of atrial fibrillation will go a long way to supporting this ambition.Dr Roy Jogiya, Clinical Director, Cardiovascular Disease, HIN
This work was also supported by the Clinical Effectiveness for South East London (CESEL) programme for AF management and SEL ICB CVD pharmacists working with acute trust specialist pharmacists to upskill and support health care professionals to initiate and manage anticoagulation for patients within primary care.
Working together, the HIN and SEL ICB were able to deliver this project to reduce the risk of heart attacks and strokes. Further work is being started to continue detecting and managing AF across south east London.
For more information about AF or other cardiovascular disease prevention programmes, please get in touch.
Contact usThe Health Innovation Network, in partnership with South East London Integrated Care System and King's Health Partners, are launching the Cardiovascular Disease Prevention Decathlon, a lifestyle intervention pilot for people living with hypertension in South East London.
Hypertension, alcohol, tobacco, obesity and mental health, also known as the Vital 5, are key drivers for health inequity, alongside wider determinants of health and psycho-social factors. In addition, hypertension is a key risk factor for heart disease, kidney disease and stroke. At present, in south east London (SEL) of those with known blood pressure aged 79 years and under, only 60 per cent have controlled blood pressure.
Hypertension can be improved with lifestyle change and medication. A small drop in blood pressure can lead to a large reduction in cardiovascular risk. However in SEL, there are no commissioned lifestyle intervention programmes for people living with hypertension.
To address this health inequity and the gap in hypertension self-management interventions, SEL Integrated Care System (ICS) and King’s Health Partners’ (KHP) have funded a pilot of the Cardiovascular Disease (CVD) Prevention Decathlon Programme. This pilot offers lifestyle intervention for people living with hypertension in SEL.
The CVD Prevention Decathlon is a 10-week structured education programme. It aims to support people living with hypertension to reduce their risk of CVD by improving blood pressure control and other heart related risk factors. The programme includes holistic wellbeing information as well as physical activity sessions and can be delivered as a face-to-face or virtual offering. Of note, the CVD Prevention Decathlon has been successfully deployed in South West London.
The Health Innovation Network (HIN), on behalf of SEL ICS, KHP, Clinical Effectiveness South East London and SEL ICS Cardiovascular Group, is seeking expression of interest (EOI) from prospective SEL primary care networks (PCNs) to pilot the CVD Prevention Decathlon programme.
In collaboration with our partners Sweat Coin, Xyla, Citizens UK, the pilot will deliver weekly 2-hour sessions, where patients will participate in teams to discover how to best reduce their risks. The pilot will include a variety of behavioural change techniques, including theory sessions, games, discussions, as well as a 45-minute physical activity session that includes a variety of sports. Patients will also have the chance to win “Sweatcoins” which they can redeem in exchange for prizes. “Sweatcoins” are also ‘earnt’ by watching weekly recap videos and participating in quizzes.
As part of the pilot, the structured education programme, delivered through partners at Xyla, is designed to help people living with hypertension:
Each week will also include an activity session delivered by a specialist sports facilitator. This will include:
The HIN, in collaboration with KHP and SEL ICS are seeking to identify PCNs interested in participating as pilot sites. A total of two PCNs will be recruited to deliver the Pilot for their population with hypertension aged 79 years and under. The pilot has the capacity of 100 spaces per participating PCN.
Before expressing interest in the pilot, please read our flyer for more details on the Decathlon.
Use the following link to submit your EOI.
Expressions of interest must be submitted by close of business on 24 November 2023.
Selected PCNs will be notified early December.
Advice and support for completing your EOI can be accessed via Claire Torkelson, Project Manager, Health Innovation Network: claire.torkelson@nhs.net.

Ensuring you've read our flyer, please express your interest to the South East London Cardiovascular Disease Decathlon.
Submit EOIRestrictive practices are techniques such as physical restraint, seclusion and rapid tranquilisation used to limit a person’s liberties, movements or freedom to act independently in potentially dangerous situations.
The inappropriate or overuse of restrictive practice in mental health services has been identified as an area of concern in healthcare since at least 2015.
Beginning in 2021, the Health Innovation Network has been involved in local efforts to reduce restrictive practice based on the findings of a successful pilot led by the National Collaborating Centre for Mental Health.
We speak to HIN Patient Safety Project Manager Ayobola Chike-Michael, Ward Manager Lola Bakare, and Expert by Experience Igoche Ikwue about the programme team’s recent visit to a female acute mental health ward and their reflections on how sharing personal experiences and perspectives are key for further reducing restrictive practice.
In my capacity as project manager for the Mental Health Safety Improvement Programme at the Health Innovation Network, I have had the opportunity to visit a few mental health wards in south London with my colleague Igoche Ikwue, who is an expert by experience.
One of the wards I was privileged to visit was Avery Ward, an acute female psychiatric ward. Despite their busy schedule, the staff welcomed us and we had the chance to meet the ward manager Lola, who later introduced us to other busy members of staff including the clinical consultant.
We had a fruitful conversation about the Ward’s approach to minimising restrictive practice. It was notable that the ward manager makes herself accessible through an open-door policy to both service users and staff. She described her unique approach as ‘we discuss, negotiate and we agree’.
This seems to be a working solution, despite experiencing the same challenge of high staff turnover which is common across these types of services. Situated in a deprived borough, the ward also faces system strain, evident in the long waiting list and pressure for beds.
Despite the dedication of staff, we learned that instances of violence and aggression affect both staff and patients. However, the team employs a range of verbal de-escalation techniques and other activities to de-escalate such as taking fresh air in the garden, and facilitating escorted leave, to manage and defuse tensions.
It was acknowledged that the pressures surrounding the ward can contribute to relapses among patients. We observed that the absence of a sensory room or equipment in the gym and the garden was in need of refurbishment. Nevertheless, plans were already underway to address these improvements and refurbish the ward.
We were told that staff experience emotional trauma from insults and violence from the service users (particularly the male staff). However, body-worn cameras have now been introduced to help take recordings of real time events.
It was evident that the staff have to daily work through a maze of challenges while trying to give quality care to the service users. We were very grateful for the open and honest conversations we had with Lola the ward manager and noted their laudable commitment to providing a safe and collaborative environment for both staff and patients.
When I arrived at the ward, I had a positive interaction with a young man who was being discharged. We had a pleasant conversation, and he expressed his excitement about returning to his music. It set a promising tone for my visit.
As I continued exploring the ward, I noticed a slight tension in the atmosphere. There was a central glass office where the staff members and administrators worked. However, it was evident that there was a shortage of staff, which understandably was causing some challenges. Despite this, the ward manager Lola demonstrated true dedication to their role, striving to provide the best care and support possible.
During our conversation with the ward manager, Ayo and I clarified that our purpose was to support the ward and its service users. We discussed several concerns, including issues with the quality of food and the need for improvements, such as the functionality of facilities. Additionally, we addressed the struggle to find bed space for service user babies as the facilities were not designed to accommodate both mother and baby. The manager also mentioned plans to relocate the facility to another building, along with a positive update on recent recruitment. There is a specialised service for mothers and babies, so patient who requires a mother and baby bed will have to be transferred out.
As someone with expertise through personal experience, I firmly believe that staff members play a crucial role in providing care and reducing restrictive practices. It is essential to prioritise the well-being of both the service users and the staff themselves. Creating a safe and open space for caregivers to express their concerns without fear of negative consequences is vital.
Despite the strain caused by system constraints, the dedication and commitment of the staff members were evident. I also observed that the ward manager maintained an open-door policy, encouraging collaboration and engagement among service users and staff.
One particular moment stood out during our visit. As we were leaving the ward, a service user approached me, expressing her strong desire to see her children. Recognising the urgency of her request, I directed her to speak with the ward manager, who promptly attended to her with responsiveness and compassion.
My experience at Avery ward highlighted the importance of providing comprehensive support and care to service users while prioritising the well-being of staff members. The ward manager and their team demonstrated a commitment to creating a safe and collaborative environment throughout our visit. I am grateful for the opportunity to contribute my expertise and be part of the ongoing efforts to improve the ward.
As a ward manager, my philosophy is that personal relationships are at the heart of creating a calm, safe and positive environment for staff and service users, where the use of restrictive practice is minimised.
I have found that building those personal relationships tends to rely on flexibility and trying to have an understanding of the whole person.
For example, I have my own ‘open door’ policy. Staff and service users can always come to me with their problems and we will do our best to figure out a solution.
Often that means negotiating; realising that both sides have to give and take in order to find a position that works for everyone.
Sometimes it is finding a way to be flexible about the small details which can make the biggest difference. Allowing more flexibility with meal times has been one way where we have seen really positive impact with service users – from a practical point of view it raised some challenges, but I am so glad we worked through them to achieve something that the people on our ward wanted.
We try and make the ward as close to home as possible, whether that means encouraging staff to make the time for escorted visits off site or building relationships with the other people who are important in the lives of our service users.
Often, we find that working with family to overcome challenges is a really effective tactic. We have multi family groups which run once a month. Family/carers and patients are invited to this meeting. Our aim is to try and create one team of people all working together for a positive outcome; that strong team is I think a big reason why we have reduced the level of complaints and of the use of restrictive practice.
Our ward – like many others – has experienced difficulties with staffing in recent years. Our staff are well trained and skilled to deliver job role. As part of my team, I have a professional nurse advocate, who provides restorative supervision for staff, and we offer monthly training days for staff.
The Ward Manager also acts as our See Think Act consultant, helping to develop relational security. This has improved the way we deliver care to our patients; our staff maintain safe and effective relationships with patients in a professional, therapeutic and purposeful way, with understood limits.
Despite the difficulties we sometimes face, I am so proud of my team; they understand how to deliver great care (including reducing the use of restrictive practice) and they are motivated and committed to continuing to get better.
For more information on our Mental Health Safety Improvement Programme, please get in touch.
Contact usLooking after the NHS is a podcast produced by the Health Innovation Network which discusses how we can make the NHS even better. Whether you are a health and care professional or simply have an interest in innovating healthcare, Looking after the NHS aims to motivate and reassure listeners that change within the health and care sector is possible.
There are over 1.5 million full time equivalent staff working in NHS in England
The theory of Dunbar’s number tells us that in our lifetime we can only maintain a stable social relationship with 150 people
The Chaos Report found that of 50,000 projects around the world, 71 per cent failed to meet these three criteria: being on time, on budget and with satisfactory results.
The podcast is hosted by Catherine Dale, Deputy Coordination Director at The AHSN Network, and Ayobola Chike-Michael, Senior Project Manager at the HIN.
In episode four Catherine and Ayo were joined by Sam Hudson, Director of Überology Ltd and recognised expert in patient participation and experience. The episode discusses Communities of Practice (CoPs), which are groups of people who share a passion for improving practice in health and care. Practitioners from different backgrounds, with different perspectives, come together across organisations and across hierarchies to meet as equals to create new knowledge and develop potential solutions to problems that go beyond what each of us can address in isolation.
Sam is currently leading the HIN and Q Network's Communities of Practice Leadership Development Programme, and was able to provide some useful insight into the real-life improvements in health and care that can be achieved through CoPs.
The impact Communities of Practice can have is really powerful. There's a kind of magic in the room when it's really in its flow.Sam Hudson, Director, Uberology
HIN Senior Programme Manager Dom Norton writes about a national programme, called the MedTech Funding Mandate, and the impact it is having on patients in south London.
At the HIN, we often work with our local hospital teams to introduce and spread the use of exciting new technologies, to ensure that everyone in south London is able to access the best in healthcare solutions. In this blog, I talk about the MedTech Funding Mandate (MTFM) which was launched by the NHS Accelerated Access Collaborative in April 2021. As we come to the end of the programme's second year, I discuss the programme, two of the MTFM innovations, and reflect on the impact they are already having for patients in south London; these technologies do not always impact large patient cohorts, but for eligible patients they can be life-changing. Lastly, I briefly look ahead to future programmes and provide suggestions on how you can help.
Case-study: GammaCore
Cluster headaches are a relatively rare type of headache, but the symptoms can be debilitating. The Migraine Trust describes them as “One of the most painful conditions someone can have.” gammaCore is a handheld device which alleviates the symptoms of cluster headaches by stimulating the vagus nerve. The treatment isn’t invasive or pharmacological and can be self-administered, unlike other treatments.
In the below video, some local clinicians from Guy’s and St Thomas’ and King’s College Hospital NHS Trusts talk about the device and the benefit it is bringing to patients’ lives.
gammaCore is now available to patients at all south London neurology centres, with more than 40 patients already having accessed this life-changing treatment option. You can access more information on gammaCore, plus an in-depth video on the device and its benefits here.
Case-study: SecurAcath
Dislodged percutaneous catheters can cause pain, infections and complications. SecurAcath is a clip that helps secure these catheters, improving patient experience and reducing the need for re-insertions.
SecurAcath is now available to patients in south London at six of seven eligible trusts, with the remaining trust in the process of introducing the clip. With the volume of clips already ordered and in use since 2020, an estimated 100,000 fewer catheter-related infections are expected, and even more hospital appointments for re-insertions are expected to be avoided. You can access more information on SecurAcath here.
One of the challenges we all face is the sheer volume of new healthcare solutions entering the market. NICE publishes guidance for over 100 new products per year, so which ones should we invest time in supporting? The benefit of national programmes such as the MTFM, with a robust product-selection processes, is that only products with the strongest evidence for effectiveness, patient benefit and cost saving make the cut.
We also know it can take a long time for newly-evidenced technologies to reach real clinical practice, and even longer to be taken up everywhere, leading to inequitable access. Our aim, through programmes like these, is to address this access gap.
The story of these first two years of the MTFM in south London is overwhelmingly a positive one: all technologies on the Mandate have been adopted by south London hospitals, and in most cases by all eligible trusts.
The really good news is that we have shown that we are able to work with partners across south London to rapidly bring new innovations into NHS hospitals; and similar success has been seen across England.
The MedTech Funding Mandate programme is now into its second round, with products supported in urology, ear, nose and throat, sickle cell disease and cardiothoracic surgery.
The department for health and social care has also recently published its first ever MedTech strategy, which highlights the important role MedTech played through the Covid-19 pandemic, and its potential for the future.
For more information, contact the AAC Programmes team on hin.nhsaac@nhs.net
Work with your local AHSN to improve access to proven innovations.
Work with us
Looking after the NHS is a podcast produced by the Health Innovation Network which discusses how we can make the NHS even better. Whether you are a health and care professional or simply have an interest in innovating healthcare, Looking after the NHS aims to motivate and reassure listeners that change within the health and care sector is possible.
The podcast is hosted by Catherine Dale, Deputy Coordination Director at The AHSN Network, and Ayobola Chike-Michael, Senior Project Manager at the HIN.
In episode three Catherine and Ayo sat down with Hazel Steele, a Matron in Medical Specialities at Guy’s and St Thomas’ Hospital and former Project Manager at the HIN. The episode discusses the importance of clinical and non-clinical roles collaborating during projects which aim to improve outcomes for patients.
Hazel, having worked in both clinical and non-clinical positions, sheds some light on how projects can be more beneficial to the needs of patients by involving nurses and clinicians in the initial scoping of projects.
“It’s all about understanding the scale of the problem at the point of delivery.”Hazel Steele, Matron, Guy's and St Thomas' Hospital

The Care Home Pioneers programme is a leadership support and professional development programme for care home leaders in south London. To date, we have supported over 70 care home managers, nurses and senior deputies on the programme, facilitating their personal growth in order to deal with the complexities of care home life.
On 7 December, the Health Innovation Network welcomed participants from the latest cohort of the programme to their graduation ceremony. The day celebrated all the Pioneers’ achievements over the course of the programme. Andrea Carter, the Healthy Ageing team’s Programme Director, reflects on the day and the importance of supporting the professional development of care home leaders.
These were the one-word descriptions given by participants and stakeholders at a recent celebration which concluded a leadership development programme for care home managers.
Care home managers became all of our heroes during the pandemic. Nightly news coverage described the challenges they faced trying to safeguard their residents, while implementing policy decisions which changed weekly, if not daily.
Over the past nine months, the Health Innovation Network, in partnership with My Home Life, has supported over 30 ‘Care Home Pioneers’ – managers leading care homes in south London. This is part of our wider programme of collaborative learning opportunities, designed to support our health and care workforce in developing technical and leadership skills and real-world improvement projects.
During the programme, we witnessed emotionally bruised staff recovering, re-committing themselves to the challenge, and striving for improvement: for themselves and their residents. The resilience and kindness of this particular group shone through and will stay with me for a long time, even after 27 years working in health and social care.
At the end of the programme the Pioneers shared their experiences and described their needs going forward.
Many described their gratitude for the ‘safe space’ that the programme provided, to discuss challenges, as well as develop creative solutions to common problems. A few explained how the programme had enabled them to secure promotion within the care home sector.
The resilience and kindness of this particular group shone through and will stay with me for a long time, even after 27 years working in health and social care. Andrea Carter, Programme Director, Healthy Ageing team
Innovation was evident. Quality Improvement projects delivered during the programme covered a breadth of topics, including how to escalate concerns to health service colleagues when residents became unwell, new ways of supporting residents to live well with dementia, and creative approaches to encourage residents to eat and drink well.
This poster presentation and video describe their achievements in more detail. Additionally, the South London Care Home Pioneer Programme 2022: Cohort 4 poster can be found here.
We’re all familiar with the extreme challenges of providing emergency care in the current climate. In London, recent data suggests that the number of care home residents represents 0.4 per cent of the population, yet accounts for around 4 per cent of ambulance conveyances and around 10 per cent of occupied hospital bed days.
Care home staff often tell us their residents do not wish to be taken to hospital, and it is vitally important that we get our escalation response right for residents, as well as for the wider system.
To achieve this, continued dialogue with care home leaders is vital. They understand the factors that come into play when determining how an unwell resident can receive the right care in the right place at the right time, including how to ensure their residents don’t suffer the indignity of death in an unfamiliar place.
Care home leaders need to be able to share their wisdom as true partners in delivering health and social care. Let’s not forget the knowledge amongst this group of leaders, and all strive to ensure that we embrace the opportunities afforded by Integrated Care Systems and Local Care Partnerships by properly engaging them in local debate.

For more information about the 2023 Care Home Pioneer Programme, please get in touch.
Contact us
Restrictive practices are techniques such as physical restraint, seclusion and rapid tranquilisation used to limit a person’s liberties, movements or freedom to act independently in potentially dangerous situations.
The inappropriate or overuse of restrictive practice in mental health services has been identified as an area of concern in healthcare since at least 2015.
Beginning in 2021, the Health Innovation Network has been involved in local efforts to reduce restrictive practice based on the findings of a successful pilot led by the National Collaborating Centre for Mental Health.
We speak to HIN Patient Safety Project Manager Ayobola Chike-Michael, Practice Development Nurse Nokuthula Marks, and Expert by Experience Igoche Ikwue about the programme team’s recent visit to an acute psychiatric mental health ward and their reflections on how sharing personal experiences and perspectives are key for further reducing restrictive practice.
As a patient safety project manager, I know how important it is to involve people and communities in shaping health and care services. The experiences of service users and carers make them experts in their own right and they should be viewed as equal partners – “Experts by Experience” – in improving services and treatments alongside healthcare professionals.
We have worked with Experts by Experience as part of our Reducing Restrictive Practice Quality Improvement Collaborative throughout the project.
Personal perspectives are always enlightening for people like me tasked with helping services to improve, but the insights that have been shared during this project have – being truthful – been emotionally challenging.
Some service users have recounted their experiences of restrictive practice with words like ‘powerless’, ‘dehumanised’, ‘traumatic’ or even ‘haunted’. These words evoke painful, negative experiences and feelings of being actively hurt by the very health and care system that is designed to keep them well.
With these raw emotions in mind, I was nervous about what our planned visit to a local mental health ward might entail.
My experience visiting the ward
During our visit, we met the Ward Manager, some members of staff and inpatients on the ward.
We spoke with the Ward Manager, Nokuthula, for over an hour, opening our eyes to the complex nature of the multidisciplinary team operating at the service and their efforts to look after people living with a range of mental health conditions.
We were taken on a tour around the ward to gain a better feel of how the dynamics of the ward came together; it was positive to see so much interaction between service users and staff.
The atmosphere was calm and peaceful. We observed some service users watching TV, some in the activity room and others in their rooms. We asked many questions as we walked around the ward – not least why anyone would be restrained at all in such an environment.
The ward manager shared some of their own successful change interventions which helped keep the use of restraints low. They talked us through initiatives such as the use of safety pods and the Bröset checklist for risk assessments. An important theme was reflection and evaluation – taking time each month for staff to consider and assess their use of restrictive practices in order to reduce them where possible.
We also talked about how important it was for both staff and service users to be encouraged to share their feelings about life on the ward. Personal relationships based on trust and understanding are vital for everyone involved in the service.
Restrictive practice is a complex issue and does not have one solution.Nokuthula Marks, Ward Manager
Reducing restrictive practice is a complex challenge, but the visit brought home to me that many of the practical interventions making a difference really boil down to doing more to understand and be compassionate towards the people involved, whether through motivating staff and providing staff wellbeing programmes, or creating a psychologically safe environment on the ward through looking at the physical space or ways in which people communicate.
I’ve spent eight years as a mental health nurse, and more than two-and-a-half as a Ward Manager. Working in acute inpatient settings is something that has always appealed to me; we see people who are very unwell and who have complex care needs, but showing the difference care and compassion can make to their recovery is incredibly rewarding.
Reducing restrictive practice is something that I think everyone involved in delivering mental health care wants to work towards, and over the past two years it has been a real focus for me personally.
The reality of working on a ward does mean it can be difficult to maintain perspective on restrictive practice. It takes conscious effort to avoid becoming “institutionalised” and treating interventions such as medication as being the only option. That is why projects such as the Reducing Restrictive Practice Quality Improvement Collaborative are so valuable – they allow for sharing best practice beyond our busy “day-to-day” lives, allowing us to gain inspiration and confidence from how other people are taking on this big, difficult challenge.
My experience welcoming Ayo and Igoche to the ward
I understand that the view many people have of acute inpatient mental health wards can be quite negative. People worry that these are chaotic, dangerous places. That is why I love having the opportunity to show people first hand the hard work that goes in to making them a positive environment and a place that helps people to recover.
It was so nice to speak with Ayo and Igoche about life on our ward. We shared insights on the approaches that have worked for us such as de-escalation techniques and spotting the early signs of distress to allow for early interventions. We also discussed specific tactics which have helped to make a difference on our ward such as the safety cross, a visual tool for recording uses of restrictive practice and prompting us to think about how we might be able to reduce them going forward.
A common theme for making progress in reducing restrictive practice is building time for reflection into our work. On the ward that can mean scheduling regular time for multidisciplinary team staff to come together in “safety huddles” to discuss recent instances of restrictive practice. In some ways the ward visit itself was an extension of our commitment to reflective practice, and I hope our experiences can aid those working in other services.
I believe that my experiences can be used to help improve mental health services.Igoche Ikwue, Expert by Experience
Reducing restrictive practice is a journey and we still have a long way to go. Our ward is continuing to work hard to be the most supportive environment it can be for our service users; we have just moved to a new, brighter location, which our service users are enjoying. We have also invested in training in “See Think Act” relational security to enable us to use the knowledge and understanding that we have of our patients and apply this to planning and providing care.
As long as we strive to communicate and collaborate, I am confident we will keep on making positive progress in reducing restrictive practice.
My experience of caring for a family member who was suffering from poor mental health was very challenging. I was isolated in my own home and it put immense strain on my own health; it was the most difficult time of my life. It makes me sad as I reflect back and recall the lack of support that I needed in times of crisis.
However, I believe that my experiences can be used to help improve mental health services – which is why I am a part of the Reducing Restrictive Practice Quality Improvement Collaborative.
My experience visiting the ward
Like Ayo, I was anxious as I walked through the door of the acute psychiatric ward we were visiting. Despite being an expert by experience, and wanting to help reduce restrictive practice, I had no idea of what to expect.
With that in mind, I was pleased and relieved that common themes running through our conversations on the ward included compassion, kindness, and humanity. We talked at length about the importance of listening and learning from service users.
My time speaking to service users and staff on the ward also made me think about my own experiences. Most service users on the ward have their own families and homes, and in many cases they will have sole carers who can be put under huge strain by the demands of looking after very unwell people. The support on offer from these services needs to extend to families – or else we risk a vicious cycle of mental ill-health and people having to spend more time as inpatients than they should need to.
The visit also gave me insight into the personal connections that underpin services, and how we could seek to improve them to reduce restrictive practice and enable better care for service users.
Whilst staff on the ward seemed to value personal relationships, I wondered if more could be done to “close the gap” between operational staff and senior leaders; understanding service user stories and experiences is of benefit to everyone and should inform decisions being made at all levels.
In the same vein, what else could be done to support staff to develop themselves and bring their best selves to work?
I was particularly struck by our discussions with Nokuthula about staff struggling with being assaulted by service users, and we discussed the importance of consistently and appropriately supporting staff wellbeing.
Personal relationships based on trust and understanding are vital for everyone involved in the service.Ayobola Chike-Michael, Project Manager, Health Innovation Network
Mentoring is another good way to help motivate and inspire staff and provide them with personal support to help to develop their confidence and willingness to try new things.
I also think more should be done to build confidence and skills in communication between team members. For example, activities like lunch-and-learns that showcase hidden talents and hobbies may be helpful, allowing team members to bond over shared or new interests. From my experience teams that engage in fun activities together have a stronger sense of trust and transparency.
Restrictive practice should always be a last resort. My visit to a ward reinforced that focusing on building understanding between staff and service users is really important in making sure it truly remains only a last resort – I hope that more effective communication, engagement and co-production of solutions between everyone involved in inpatient mental health services will continue to reduce its use.
This project is featured in our Annual Report 2022/23.
Find out more about this project in our Annual report 22/23.

It’s been a busy year at the Health Innovation Network, from publishing new reports on digital health inequalities and diabetes care for mental health inpatients, to starting new workforce development programmes for cardiovascular disease and opioids, through the launch of our new involvement strategy and supporting over £600,000 to pilot new automation solutions.
With more people living with dementia, it’s important that care home leaders feel well equipped in supporting those living with it. Dr Caroline Chill, the Clinical Director for the Healthy Ageing Programme at the Health Innovation Network (HIN), spoke at the 16th UK Dementia Congress in Birmingham on how we can use leadership development to improve care for people living with dementia.
At the HIN, helping develop skills of those working in the health and care systems is one of our top priorities. Our flagship programme aimed at professional development in the care sector is the South London Care Home Pioneers Leadership Programme, facilitated in partnership with My Home Life England. Having recently completed its fourth cohort, the programme has helped over 70 care home managers and senior staff across south London to develop their skills, share learning and become champions for improving dementia care in their local area.
Dr Chill used the presentation to explore the Service Improvement Projects, which Pioneers undertook as part of the programme within their homes, many of which focus on care home residents living with dementia. To celebrate the work that the senior care home staff have been doing, we interviewed, and filmed two Pioneers from care homes in Bromley: Natasha Leslie and Nicola Orme. Nicola focused on helping relatives understand more about dementia while Natasha explained how she had introduced activities to respond to ‘sundowning’ – a period of agitation commonly experienced by people living with dementia in the late afternoon.
Nicola found that families’ understanding of dementia had increased following her Service Improvement Project, scoring on average 3.0 on a pre-workshop questionnaire and 4.75 post-workshop. Natasha also reported residents felt more supported and engaged in activities, with fewer incidents in the care homes such as falls and behaviours of concern. This had a knock-on effect with fewer 999 and 111 calls. Both projects have made a difference in the quality of care for residents, as well as a reduction in complaints and improvement in relationships between residents, staff, and their families. You can watch the full interview below.
“Presenting at the 16th UK Dementia Congress was a great opportunity to showcase the achievements of care home staff and to demonstrate the importance and value of quality improvement work in care home settings.” Dr Caroline Chill, Clinical Director, Healthy Ageing, Health Innovation Network
The South London Care Home Pioneers Programme is a leadership support and professional development programme delivered to Care Home Managers, Deputies, and Senior Nurses to advance their skills, facilitate personal growth and help them manage the complex everyday issues that impact on the quality of their service. The programme consists of a combination of four workshops, three which cover the managing of self, others, and change, and one service improvement workshop. Additionally, participants on the programme undergo nine monthly action learning sets, which involve experiential learning through a continuous process of action and reflection, supported by colleagues. The Pioneers on the programme also benefit from working alongside mentors from the HIN, who provide support to deliver a service improvement project within their care homes.
If you would like to learn more about dementia, and understand how it affects the brain and memories, take a look at this video from Dementia UK. Alternatively, if you are interested in learning more about the Care Home Pioneer Programme and how it can support leaders to deal with the complexities of dementia, please get in touch.
If you would like to find out more on the Care Home Pioneers programme and our work supporting people living with dementia, please get in touch.
Contact usHundreds of thousands of people in the UK experience painful slow-healing lower leg wounds such as ulcers each year.
A new collaborative project led by the Health Innovation Network (HIN) and Bromley Healthcare Community Interest Company (CIC) hopes to test evidence-based approaches to transforming care for these types of wounds, with the aim of improving the quality of life for patients and reducing costs to the NHS.
The AHSN Network Transforming Wound Care national spread and adoption programme aims to ensure all patients with lower limb wounds receive evidence-based care. This leads to:
The programme uses the evidence, learning and recommendations from the National Wound Care Strategy Programme (NWCSP).
The Health Innovation Network, the Academic Health Science Network (AHSN) for south London, is taking part in Phase 1 of the programme and is supporting Bromley Healthcare CIC to establish a dedicated Lower Limb Wound Clinic Test and Evaluation Site.
Most wounds to lower limbs heal within a few weeks. Chronic lower limb wounds are those below the knee that are slow or fail to heal. Chronic lower limb wounds account for at least 42% of all wounds in the UK, with leg ulcers being the most common type (34% of the total wound population, compared to 7% pressure ulcers and 8% diabetic foot ulcers).
A large proportion of the total wound care spend is for these chronic lower limb wounds because of their slower healing rates. In 2019, there were an estimated 739,000 leg ulcers in England with estimated associated healthcare costs of £3.1 billion per annum year.
Based on evidence from the National Wound Care Strategy Programme, the prevalence of total leg ulcers is expected to increase by around 4% annually, to over 1 million by 2036 if there is no intervention. This is driven by an increase in leg ulcers that either recur after healing or those that do not heal.
“Bromley Healthcare is delighted to be selected as a pilot Test and Evaluation Site for the new national Transforming Wound Care programme. The national wound care strategy will significantly reduce healing times for people, provide a better quality of life and maximise our nursing time. We feel honoured to be part of such an important programme working to improve wound care for people closer to home.
As a community service provider for people in South East London, we work closely with GPs and acute colleagues to ensure wound care is joined up. Through becoming a Test and Evaluation Site, we look forward to strengthening our joint work to support the early identification of wounds and continue to build our shared knowledge to improve care for people with wounds” – Jacqui Scott, Chief Executive Officer, Bromley Healthcare
The three key elements of the programme are:
Find out more about the national programme.

As DigitalHealth.London’s Accelerator programme is recognised for its role in supporting innovators, we reflect on the vital importance of AHSNs and their partners in helping the patients and the wider health and social care system benefit from commercial innovation.
On 7 July, DigitalHealth.London’s Accelerator programme was selected as winner of Accelerator of the Year award at the UKBAA Angel Investment Awards 2022. We are delighted that this award recognises the impact and importance of collaborative working by Academic Health Science Networks (AHSNs) to help innovators bring their digital health solutions to bear against some of the biggest challenges facing the NHS.
The DigitalHealth.London Accelerator is a highly competitive 12-month programme for digital health companies that have products or services with high potential to meet NHS and social care challenges. High potential SMEs undertaking the programme are given bespoke support and advice, expert-led workshops and events to broker meaningful connections between innovators and NHS organisations.
The programme is delivered by Health Innovation Network and UCLPartners, MedCity and Chelsea and Westminster Hospital Charity (CW+), and has benefited from AHSN funding from NHS England, the Office of Life Sciences and Greater London Authority ERDF. The delivery of the Accelerator programme has connected industry, academia and the NHS to exchange ideas and collaborate to support innovation and the adoption of digital health.
“I am extremely proud to see the DigitalHealth.London Accelerator being recognised as pivotal programme, supporting high potential innovators to tackle health challenges within the complex NHS market. Being selected as winner of Accelerator of the Year award is a fantastic achievement that reflects the collaborative efforts of everyone involved across the London AHSNs and our partners.”Anna King, Commercial Director, Health Innovation Network
With the NHS under continued pressure following the Covid-19 pandemic, innovative solutions are already proving crucial for tackling issues such as the elective care backlog and widespread workforce challenges, with new approaches also helping to counteract existing health inequalities.
Beyond its positive impact on patients and NHS services, the Accelerator is also a significant catalyst for economic growth in the capital.
In the six years since its inception, the Accelerator has supported 143 digital health companies and 591 new contracts have been secured by these companies because of Accelerator support. The companies on the Accelerator have created a gross total of 1,498 new jobs during the programme and 45 new products have been launched to the NHS market.
Get in touch to find out more about DigitalHealth.London and their Accelerator programme.
Contact us
This news story relates to the 2022 CVD Fellowship. Click here to find out about the 2023 CVD Fellowship.
Over 100 clinicians working in primary care in south London have today (Monday 21 March 2022) been welcomed on to the Health Innovation Network’s (HIN) first ever Cardiovascular Disease (CVD) Prevention Fellowship.
This free HIN programme is designed to help improve outcomes for patients across south London who are at risk of CVD by supporting clinicians working in primary care to develop their skills and knowledge and champion CVD prevention in their practice or wider Primary Care Network.
In total there are 104 Fellows who are either pharmacists, GPs, practice nurses or physician associates. From Richmond to Bexley all 12 south London boroughs are represented and Fellows come from a range of backgrounds and are representative of the communities they serve.
The programme will provide free expert clinical advice and quality improvement support to help Fellows become CVD prevention champions. It will also help them identify and implement specific local CVD prevention initiatives in their practice and local area.
With six million people living with CVD in England with a combined cost of £16 billion every year improving outcomes for at risk patients is an NHS priority. This programme will help to speed up the adoption of innovative initiatives to help prevent CVD across south London.
Applications to the programme have now closed.
Dr Roy Jogiya, Cardiovascular Disease Prevention Clinical Director, Health Innovation Network, said:
“It gives me great pleasure to welcome over 100 clinicians to our first ever Cardiovascular Disease Prevention Fellowship. This is an exciting learning opportunity that will include teaching from a number of national experts in cardiovascular disease. This will empower Fellows to be up to date in their knowledge base and feel more confident in managing cardiovascular disease prevention within their community of pratice.”
Oliver Brady, Programme Director for CVD Prevention, Health Innovation Network, said:
“It is fantastic that so many clinicians from a wide variety of backgrounds applied to be Fellows. And it is great that every borough of south London is represented on the programme. We will support these Fellows to champion cardiovascular disease prevention in their local area and together we have the opportunity to make a real difference to people who are at risk of cardiovascular disease.”
Running from April to October and culminating with a graduation ceremony in November the programme will consist of six monthly lunch time webinars led by experts in a range of areas including lipid management, hypertension and atrial fibrillation. There will also be ongoing Improvement Collaborative sessions and peer to peer networking opportunities.
For more information about our Cardiovascular team and the CVD Prevention Fellowship Programme, please get in touch.
Contact us
In our latest blog Rayvathi John, Health Innovation Network People Lead, reflects on how we get the recruitment process right and what is important in the hiring process in an ever competitive employment market.
Getting recruitment right, for every post, it is crucial to ensure not just that our important work is completed to a high level, but also that we engender the right culture at any organisation. A lot has changed in the way we hire and onboard our new starters at the Health Innovation Network (HIN) over the last two years. We have made some significant changes, and I am keen to share some of my experiences.
As People Lead, there are two questions I ask myself when it comes to recruitment.
The first is what is important in the hiring process? Is it simply finding the right candidate who can do the job or appointing the right candidate through a fair process which is without any hiring biases? NHS appointments and recruitment systems are robust and compliant with the Equality Act. This helps mitigate some of the issues of unfair practices at the application stage.
The second question is how can we attract the right candidates? How can we be the employer of choice? Gone are the days where it was the employer’s market. With globalisation and the HIN being located in the capital of the country, it is important to be competitive in the employment market. This is getting harder for the NHS as the demands of the workforce have changed and many more employers are also offering great pension schemes and improved work life balance schemes. So, how can we sell and promote our job roles to attract the right candidate where we have limitations in what we can offer to the candidate? How can we seek the best candidate from across the sectors to make NHS teams reflect with wider experience?
So what does attract candidates?
According to Hays’ data, 62 percent of professionals would be willing to take a pay cut for a job with more purpose. “Money is important, but it’s about having that compelling purpose and visions,” says Cathy Donnelly, Sr Director, Talent at Liberty IT. “We need to help people understand the difference they can make.” We are fortunate at the HIN that our jobs do have purpose and make a difference to NHS staff and patients and innovators in south London and we need to demonstrate our understanding of that. For example some of our latest projects have demonstrated the value that remote consultations, teledermatology, and virtual wards can add.
This is why it is vital during interviews that we promote the projects the HIN undertakes and the impact they have on the lives of patients and society – did you know that one of our Innovation Grant funded projects provided health checks for 441 people across six health clinics at local Black Caribbean and Black African Churches, a Tamil template and two mosques? We need to ‘recruit with reputation’ by emphasising our values of being kind, brave, open, together and different, so candidates are able to feel the culture as well as the work we deliver.
We were able to put this into practice in 2020 and 2021 when we had a number of business-critical appointments in the organisation, including a new CEO and a Chair. The process for the appointment of the CEO and Chair was intense but with a clear expectation that we wanted to appoint based on merit with equality of opportunity for all. Jobs were advertised externally on NHS jobs, NHS Executives, LinkedIn and Twitter for maximum coverage.
We engaged with stakeholders who know how the HIN operates and how the success of the appointment would be measured, including using our key external stakeholders, Board members, diverse panels and our host organisation. As with all recruitments, there was a need to balance conducting an efficient process but making sure the right candidate was appointed so that there was not an adverse impact on the HIN’s performance.
Having been a candidate using NHS Jobs or Trac to apply for a vacancy, I have at times felt extremely frustrated trying to complete the online application form. I am sure all the applicants who applied to the role of the CEO and Chair might have felt the same frustration. While the application process can still do with some improvement, the improvements to the anonymous shortlisting and online working have helped make the process run more smoothly and is a practical step to protect against bias.
We are a great place to work and we invest a lot of time getting our recruitment right. As we continue our journey towards becoming an outstanding organisation, we will be focusing on improving the responsiveness of our services, and looking for innovative ways to further promote equality, diversity and inclusion in our recruitment process.
If you would like to share your innovative ways of recruitment or if you need more information on our processes, please feel free to connect with me at rayvathi.john1@nhs.net.
Reference:
www.peoplemanagement.co.uk/long-reads/articles/how-be-employer-choice-talent-attraction-retention

Catherine Dale, HIN Programme Director for Patient Safety and Experience and Sophie Lowry, Implementation and Involvement Manger, provide an update on the HIN’s Involvement Strategy – also a key theme of lively discussions in episode 2 of our Looking After The NHS podcast series now available for listening.
Catherine Dale reflects on episode two of our Looking After the NHS podcast:
“The mechanic doesn’t ask me where they need to put the fanbelt. So why should healthcare experts, who have trained for years, have to listen to someone else?”
Ayo Chike-Michael and I get to grips with this issue in Episode 2 of our podcast series ‘Looking After the NHS’ which I am delighted to say you can now listen to below.
In this episode we are joined by Cristina Serrão – Lived Experience Ambassador in the Experience of Care Team at NHS England and Improvement. If you want to find out the answer to this question – give it a listen.
We have a great discussion about how involving people in the design and development of services can make the NHS even better. We cover a range of topics including why we should involve patients and what co-production actually looks like in reality. We also grapple with a range of challenges around involvement and consider the benefits, including reducing health inequalities.
I loved recording this episode, Cristina has a real wealth of insights and her passion for involvement is truly infectious! Involvement really is a real priority for me and for the HIN, and I hope this episode brings to life why it is such an important topic for us to address.
Sophie Lowry provides an update on the HIN's Involvement Strategy:
Over the last few months Catherine and I have been working with colleagues and people who live and work in south London to develop the HIN’s Involvement Strategy. We heard:
“No one person, no one part of the system knows the 'right' answer.”
“Patients are people who are more than their condition and diagnosis.”
“You can’t do innovation without involvement.”
Well, here at the HIN we wholeheartedly agree with all of these statements.
This week we brought together some of the people who have contributed to our Involvement Strategy to update them on the progress we have made and also to gather feedback on our emerging approach and delivery plan. This was the first opportunity we had to meet some people in person, and we felt such a buzz being able to socialise in person and use real post-it notes! We were also able to trial a “hybrid” approach, with some people dialling in to join in the discussion. It provided a great opportunity to connect, and our Chief Executive Rishi Das Gupta was able to thank people first hand for their insights, ideas and experiences that are centre stage of our Strategy.
We were delighted to hear that there was broad consensus that we have the basis of a strong strategy, one that will make a real difference to the way which we work and to the impact we have on local health and care systems. We were also pleased to hear that people were encouraged by the fact they could see the outputs from the workshop feeding into the strategy.
You may be asking “why does the HIN need an Involvement Strategy”? Well, we want to build on the HIN’s history of involvement and co-design activity and create a more embedded and consistent approach. We truly believe that the best way to achieve the HIN’s mission to ‘speed up the best of health and care together’, is to work in partnership with people in south London. As we believe that, by sharing their insights and knowledge, people with lived experience of health and social care services can help us to improve and innovate health and social care.
That is why this strategy, and the plan that will deliver it, has been co-developed with people with lived experience, HIN colleagues, other partners and stakeholders (over 65 people in total). We have had some incredibly open and honest discussions looking at both the psychological and practical barriers to involvement and how they can be overcome. And we believe that this transparency has been vital in developing a meaningful strategy that will make a genuine difference.
Catherine and I are so grateful for everyone’s ongoing support in helping to get this right. We will now work to finalise the Strategy and look forward to publishing it shortly and working with our colleagues, both at the HIN and wider, to put it into practice!

The Health Innovation Network has launched a new Cardiovascular Disease (CVD) Prevention Fellowship Programme to develop clinical skills and knowledge to help improve outcomes for patients across south London who are at risk of CVD.
This free programme is the first of its kind and is aimed at nurses, GPs and pharmacists working in primary care in south London who are keen to develop their skills and knowledge and champion CVD prevention in their practice or wider Primary Care Network.
It is Continuing Professional Development (CPD) accredited and will provide free expert clinical advice and quality improvement support to help fellows become CVD prevention champions. It will also help them identify and implement specific local CVD prevention initiatives in their practice and local area.
Running from April to October 2022 and culminating with a graduation ceremony in November the programme will consist of six monthly lunch time webinars led by experts in a range of areas including lipid management, hypertension and atrial fibrillation. There will also be ongoing Community of Practice sessions and peer to peer networking opportunities.
With six million people living with CVD in England with a combined cost of £16 billion every year improving outcomes for at risk patients is an NHS priority. This programme will help to speed up the adoption of innovative initiatives to help prevent CVD across south London.
Applications for the programme have now closed.
“We are delighted to launch our first ever CVD Prevention Fellowship Programme. Our free programme will be delivered by experts in their field and will arm clinicians with the knowledge, skills and confidence they need to drive forward innovative schemes and make a real difference to patients at risk of CVD in their area.”Oliver Brady, CVD Prevention Programme Director, Health Innovation Network
Get in touch for more information about our CVD team and their projects
Get in touch
The Health Innovation Network and My Home Life are delighted to announce the fourth Care Home Pioneer Programme – a leadership support and professional development programme delivered FREE of charge to Care Home Managers, Deputies, and Senior Nurses to advance their skills, facilitate personal growth and enable them to effectively manage the complex everyday issues that impact on the quality of their service.
The ‘Pioneers’ programme is a collaboration between My Home Life England and Health Innovation Network, which has delivered leadership development to 44 care home managers across South London, over 3 cohorts since 2017.
The Care Home Pioneer Programme will use Action Learning techniques which involve experiential learning through a continuous process of action, learning and reflection, supported by colleagues, with an intention of improving practice. The Pioneers will also work alongside mentors from the HIN to deliver a service improvement project within their care homes, such as reducing falls or improving oral health.
The FREE programme is jointly funded by care home commissioners and the NHS, and will consist of a combination of four workshops and nine monthly action learning sets. At the end of the programme, there will be a graduation day to celebrate all that has been achieved and to welcome you into the Pioneer Alumni.
This infographic highlights key feedback from Pioneers who took part in the programme from 2020-2021.
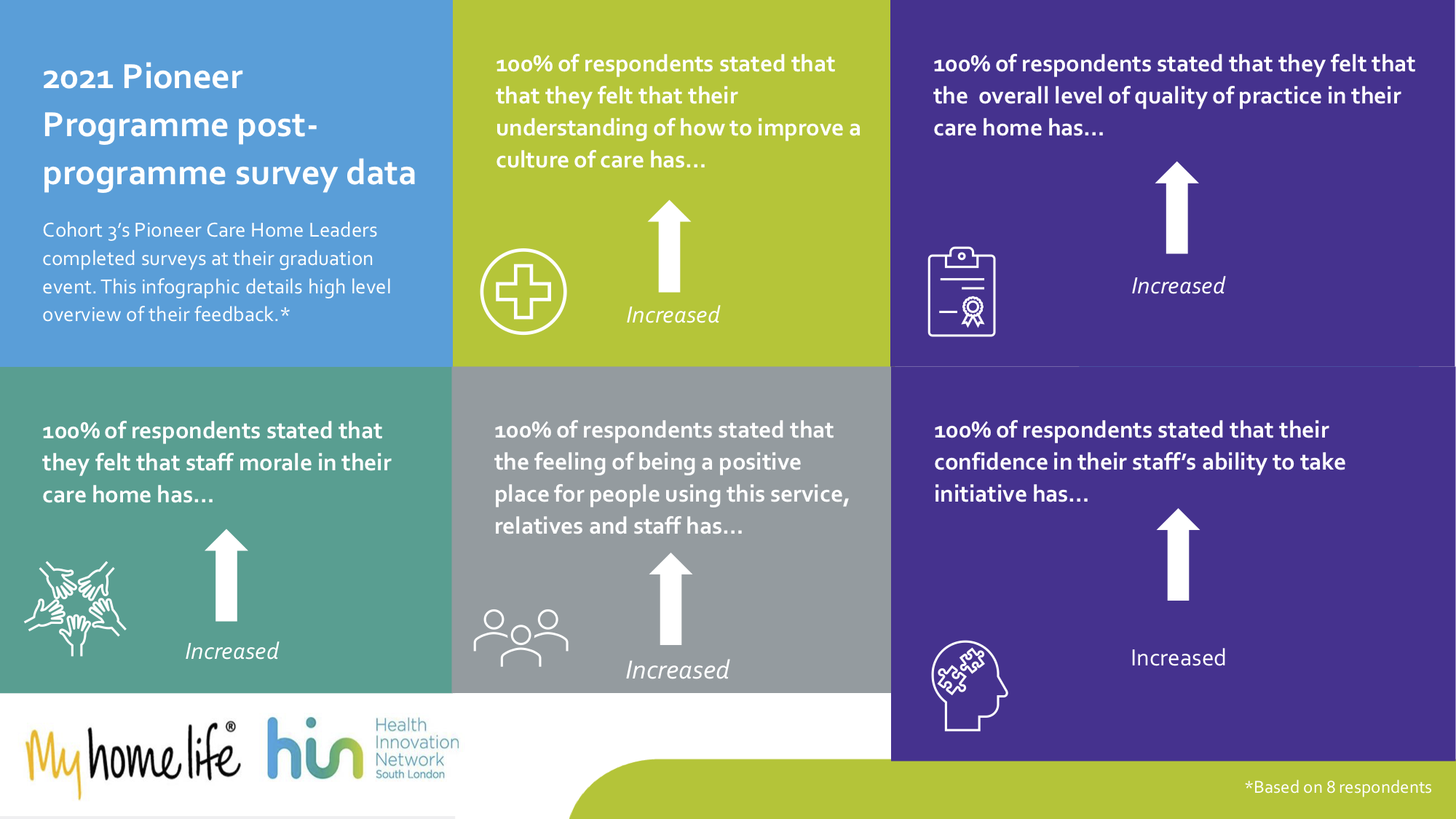
Pioneer, Cohort 3, Care Home Pioneers, said: “It’s not a training programme. We are learning from one another. The impact of it has given me a huge amount of confidence to deal with things differently.”
Pioneer, Cohort 3, Care Home Pioneers, said: “I have introduced daily team meeting with the nurses which has helped to boost self-esteem as they are able to discuss any difficulties they may have in their work”
George Croft, Healthy Ageing Project Support Officer, Health Innovation Network, said: “The feedback from the Pioneers shows that the programme has played an important role in supporting care home managers during the toughest times that the sector has faced in its history, arming leaders with an array of skills and confidence to engage with wider clinical services to help keep residents safe.”
Get in touch for more information about Cohort 4 of the Care Home Pioneers programme.
Get in touch
Cohort 3 of the Care Home Pioneer programme took place amidst the backdrop of the coronavirus pandemic, meaning that all the programme’s sessions were held via Zoom. As a result, the graduation event presented an opportunity for the Pioneer care home leaders to meet in person for the first time. George Croft, the Healthy Ageing Team’s Project Support Officer, reflects on the day.
The Pioneer programme has graduates represented across all the south London boroughs.
14 Care Home Managers started Cohort 3 of the Pioneer programme, 9 of whom went on to take part in the Quality Improvement workshops.
100% of Pioneers who completed the final session feedback survey reported the skills that they learned as part of the whole programme were useful and effective in their everyday role.
On Tuesday 2 November, the Health Innovation Network (HIN) and My Home Life came together at Southwark Cathedral to celebrate the achievements of the third cohort of south London Care Home Pioneers. The Pioneer Programme is a leadership development programme for care home managers and senior care home nurses based in south London. The HIN has run the Pioneer programme since 2018 in partnership with My Home Life, an organisation working to support quality of life for all people who live, die, work and visit in care homes.
When I joined the HIN in March 2021, I was excited to witness first-hand how the HIN’s work impacted the lives of people working “on the ground” in health and social care. My time so far supporting the Pioneer programme has proven to me the value that projects like ours can bring to the care sector and those who work within it.
At the graduation event, seven Care Home Pioneers joined us to not only celebrate their achievement of taking part in the programme but also to acknowledge the strength and compassion that they demonstrated whilst caring for their residents during the coronavirus pandemic. The Pioneers reflected that the Action Learning sessions fostered a “wellness space” as well as a way of “checking out of work and checking in with colleagues” for a few hours every couple of weeks. One care home manager explained passionately that the sessions were “where I would go to recharge my batteries, they gave me courage during difficult conversations” – a remark that has stuck with me in the weeks after the event.
Care home staff have long felt undervalued in comparison to their NHS colleagues [recently highlighted in BBC One’s Inside the Care Crisis with Ed Balls] and the Pioneer programme is one way that we can help arm leaders with a “portfolio of tools” as one Pioneer put it. Another care home manager mentioned that the programme helped her “learn how to delegate better, helped my home develop shared decision making, and hand more responsibility to staff, which reduced my stress and helped me gain a better work/life balance.”
The Action Learning component of the programme was led by My Home Life facilitator Danuta Lipinska, who commented – “I certainly felt quite emotional, not only to meet these hardy Pioneers, but to be reminded of what they had all endured and survived, and were now thriving, even though the Covid-19 virus is still with us… We celebrated the achievements of these dedicated and selfless women and men and applauded loudly as we awarded well deserved certificates to the Pioneers. We wish them continued success and stamina in the months that follow, safe in the knowledge that they are not alone and have forged strong relationships with one another and are Associates of the My Home Life and HIN community – a compassionate, skilled and formidable presence in south London.”
When the Pioneers signed up for the programme, none of them expected to be taking part in virtual workshops, with all the demands that being a care home manager brings erupting in the background. Whilst helping deliver the HIN’s quality improvement element of the programme over Zoom, it was clear to me that there were a lot of exhausted faces in the room, even after the peak of the pandemic. Cohort 3’s graduates told us that whilst the programme would have been better delivered face-to-face (which the HIN would traditionally do), a hybrid of some virtual sessions would also be helpful on occasion for future cohorts.
“The feedback from the Pioneers shows that the programme has played an important role in supporting care home managers during the toughest times that the sector has faced in its history, arming leaders with an array of skills and confidence to engage with wider clinical services to help keep residents safe.”George Croft, Healthy Ageing Project Support Officer, Health Innovation Network
Whilst covid restrictions have been lifted, significant challenges remain for care homes. The existing workforce issues have been elevated further by staff burnout, as well as the government’s announcement that vaccination against Covid-19 is to become a condition of deployment in care homes. However, the feedback from the Pioneers shows that the programme has played an important role in supporting care home managers during the toughest times that the sector has faced in its history, arming leaders with an array of skills and confidence to engage with wider clinical services to help keep residents safe. Working on Cohort 3 of the Pioneer programme has been a pleasure, and I look forward to future work that we can do to support alumni and future cohorts.
The HIN are in the process of securing funding for Cohort 4 of the Pioneer programme, which will be co-designed alongside alumni of previous Pioneer cohorts, to deliver a programme that best meets the needs of care home leaders in south London.
To find out more about the exciting upcoming work within the Pioneer Programme, get in touch with our Healthy Ageing team
Contact us
The Dermatology Improvement Collaborative was a bespoke quality improvement programme designed and delivered by the Health Innovation Network, Kent, Surrey and Sussex AHSN and supported by the Industry Dermatology Initiative (IDI). The programme was fully funded by the IDI and they also supported with the development of activities and outputs. The collaborative worked to support local south London and Surrey dermatology services to streamline the patient pathway and clear their backlog.
Note: a full report looking at the work of the Collaborative was published in 2023.
Pre-pandemic, the referral to appointment time (RTT) was 16 percent over the 18-week marker in south west London and 31 per cent over in south east London. Covid-19 dramatically worsened the situation as a result of Consultant Dermatologists and other operational staff being redeployed to deal with the pandemic response, therefore further increasing patient waiting times.
However, with funding from NHSX to accelerate the introduction of teledermatology in south east and south west London ICSs, the Dermatology Improvement Collaborative was able to support each ICS to implement new technology which aim to reduce wait times for patients.
The focus for south east London ICS was utilising their clinical resources more effectively, particularly in clinical triage and referral. A technology platform was implemented to manage clinical virtual review. A joint consultant rota was generated where consultants across the three NHS Trusts in south east London could review referrals before they are actioned, in order to streamline clinical triage.
In south west London ICS it was about reducing waiting times for dermatology appointments in secondary care. Educational videos were created to support patient and GP education of the treatment and management of skin conditions. As a result, GPs could make more informed decisions and therefore more appropriate referrals, which reduces wait times.
Ashford and St Peter’s NHS Foundation Trust sought solutions to address increasing service size and demand. For their two-week wait skin cancer referral pathway, they established teledermatology ‘photohubs’ across three north west Surrey locations. Employing healthcare assistants to take high quality images, which were uploaded securely to the Trust image database for review by the dermatology consultants. Next steps are to pilot the AI tool Skin Analytics in their services as part of the NHSX’s Artificial Intelligence in Health and Care Award.
“Like many across the country, Dermatology teams in south east and south west London were put under huge pressure during the pandemic, but by embracing new technology they saw the potential to improve their services. We hope the report into their success can help more dermatology services to transform their services through introduction of technology to help to reduce wait times for patients.”Lesley Soden, Programme Director of Innovation Theme, Health Innovation Network
A number of case studies were produced using the insights gathered and have now been translated into a report to share lessons learnt for all dermatology services wanting to implement teledermatology. These case studies will be being presented at the Conference: Govconnect – NHS Long Term Plan 2021 Meeting on 30th November 2021.
The IDI is a cross-industry collaboration to improve dermatology care and includes and is funded by the following member companies: Amgen, Eli Lilly and Company, LEO Pharma UK, Sanofi and UCB.
Date of preparation: September 2021 Document number: GB-NPS-0921-00004

We absolutely love the NHS. But let’s face it, it’s not perfect. Yet.